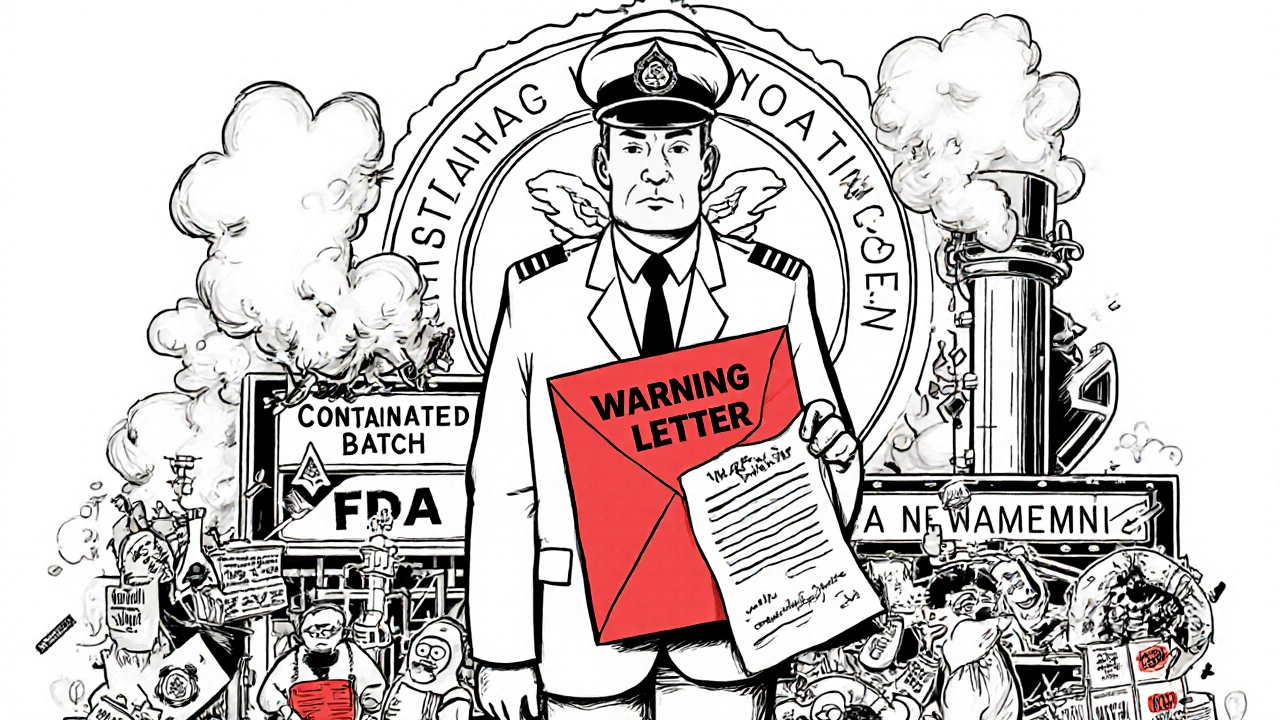
The FDA issues hundreds of warning letters each year to manufacturers who violate safety and labeling rules. Learn how these letters work, what happens if you ignore them, and how to avoid enforcement actions.
Non-Compliant Manufacturers: Risks, Red Flags, and How to Stay Safe
When you buy medication, you trust that it’s made the right way. But non-compliant manufacturers, companies that skip safety rules, cut corners, or fake quality controls. Also known as unregulated drug producers, these operators put dangerous substances into pills, creams, and injections — and they’re more common than you think. The FDA and Health Canada flag them yearly, but many slip through, especially when sold online or through shady distributors. These aren’t just small-time operators — some are large labs with fake certifications, shipping fake insulin, fake antibiotics, or even pills with no active ingredient at all.
Why does this matter? Because counterfeit drugs, fake versions of real medications that look identical but contain wrong or harmful ingredients can kill. Think of the 2022 case where fake metformin caused kidney failure in patients across three countries. Or the 2023 recall of contaminated blood pressure pills linked to a non-compliant factory in India. These aren’t rare outliers — they’re symptoms of a broken supply chain. Even generic medication risks, dangers from unverified manufacturers who change excipients or skip bioequivalence testing are real. A study in the Journal of the American Pharmacists Association found that 1 in 10 generic pills bought from unverified online sources had incorrect dosing — some with too little, others with toxic fillers. And it’s not just about potency. Bad excipients — like the talc or dyes used in some generics — can trigger allergies or interfere with how your body absorbs the drug, especially if you’re on narrow therapeutic index meds like warfarin or lithium.
It’s not all doom. The good news? You can protect yourself. Stick to licensed pharmacies, check for verified seals, and avoid deals that seem too good to be true. If a site doesn’t list a physical address, doesn’t require a prescription for controlled meds, or ships from a country with weak oversight — walk away. The non-compliant manufacturers rely on secrecy and low prices. They can’t compete with transparency. Below, you’ll find real stories and science-backed guides on spotting risky sources, understanding why drug shortages happen, and how to get safe, affordable meds without falling for scams.