When Medications Play Tricks on Your Bladder
Ever come back from a night out, flop onto your bed, and realize you’ve made more bathroom trips than actual memories? It’s not always about chugging water or your caffeine fix. If you’re on certain medications, they might be nudging you to the bathroom way more than you’d like. This isn’t something you just have to put up with—it’s real, it’s common, and it’s tied directly to what’s in your medicine cabinet. Let’s talk about what’s happening, the science behind it, and what you can actually do, because nobody likes playing musical chairs with their toilet.
Here’s the thing—your bladder and kidneys are super sensitive to chemical changes. You take that new prescription, and suddenly your bladder is working overtime like it’s got something to prove. For a lot of people, this isn’t discussed when picking up medications, but it can seriously mess with daily life—think waking up three times a night to pee, planning your route by where the nearest restrooms are, or stopping a movie because you can’t sit still for two hours. Pharmaceuticals have side effects, and increasing urinary frequency is near the top for certain popular meds.
A few classic culprits are tamsulosin, diuretics (you’ll hear them called water pills), blood pressure meds, some antidepressants, certain pain meds, and even allergy tablets. It’s not just about peeing a little more often. For a chunk of people, it’s about suddenly feeling like you can’t empty your bladder, weaker flow, or occasionally, getting caught off guard with leaks. Stats show about 30% of adults on these drugs report changes in their urination habits. But why?
Every medication has its own way of throwing your system off. Some relax the bladder muscles so much they rattle your “hold it” ability; others ramp up urine production; a few just tweak your nerves until your bladder gets mixed signals. These changes can show up fast or after a few weeks—sometimes they fade; other times, they stick around as long as you’re on the medication.
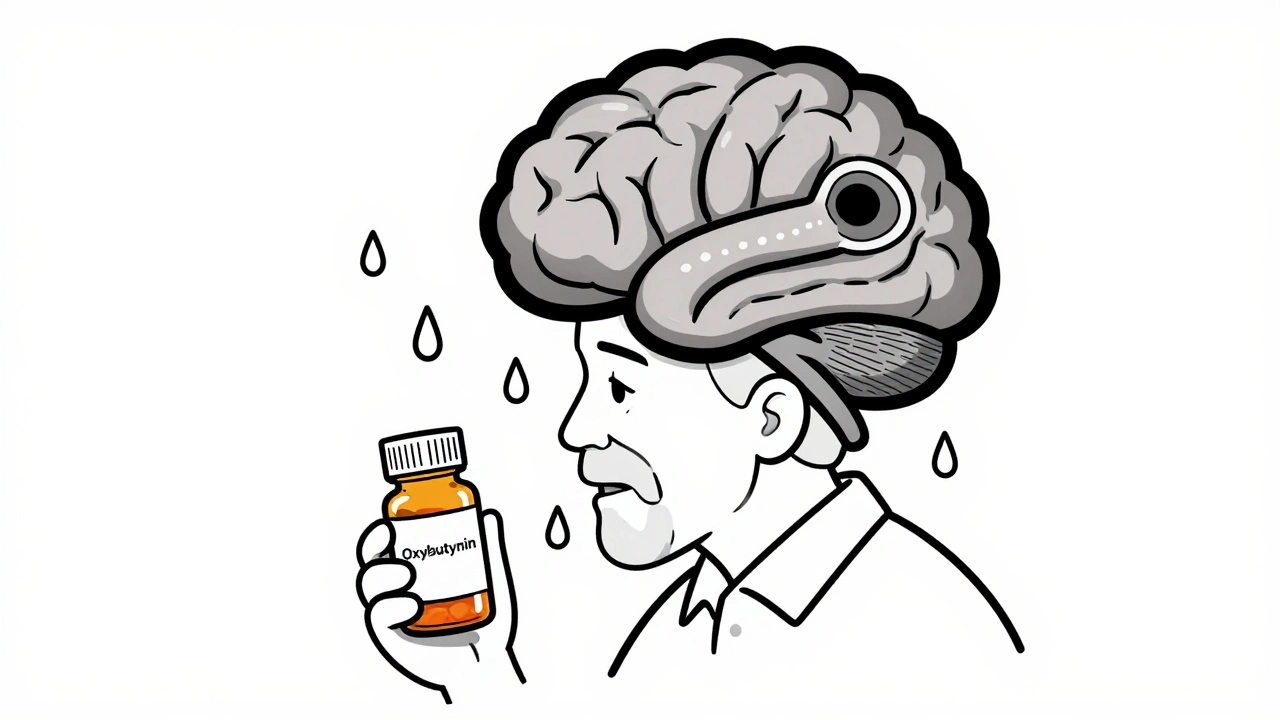
If you dig into the science, specialists will tell you that a balanced bladder depends on messaging between your brain, bladder, kidneys, and a bunch of nerves. Certain drugs play with these messages. Take alpha blockers like tamsulosin—they target the “tightness” in the prostate and bladder neck so pee flows easier. But they might tip the scales too far, making you pee more often. Then you have diuretics, which literally force your kidneys to push out more salt and water; guess where that water is going? Other meds mess with hormones or chemicals in your brain, nudging your body to make more urine or sending more frequent “go now” signals.
This doesn’t even count how your own biology can magnify the effect. Some people have bladders that are more sensitive to change. Throw in being over 50, being female, or having a history of urinary issues, and the bathroom invitations multiply.
Medications Most Likely to Make You Pee More
Let’s get specific. Knowing which drugs can spark these issues helps you talk back to your doctor, rather than just putting up with it. You might recognize some of these from your own medicine shelf or someone in your family.
- Tamsulosin (Flomax): This alpha-blocker is often prescribed for guys with enlarged prostates. Its main gig is to relax muscles around the bladder and prostate to make peeing easier. But there’s a twist—relax them too well and you might get the urge to pee every couple of hours.
- Other Alpha Blockers: Drugs like alfuzosin or doxazosin work a lot like tamsulosin, bringing relief in one way but also leaving you checking the bathroom clock in another.
- Diuretics: Water pills like furosemide, hydrochlorothiazide, or spironolactone are all about helping your body dump excess water and salt. The downside? A big spike in urine output, usually within hours of taking your dose. Some people find themselves running to the bathroom five or more times in a morning.
- Some Antidepressants: Selective serotonin reuptake inhibitors (SSRIs) and tricyclics sometimes mess with the nerves that control bladder function, making you pee at weird times or more than usual.
- Antipsychotic Medications: Again, they tweak neurotransmitters (chemical messengers) in your nervous system, leading to unpredictable bladder habits.
- Blood Pressure Meds: ACE inhibitors, ARBs, and calcium channel blockers can all have mild to moderate effects on how often you need to go, though not as much as diuretics do.
- Cold & Allergy Medications: Antihistamines can dry you out and make it tough to pee for some; decongestants can have the opposite effect, letting urine flow a little too easily.
Here’s a quick look at how common this is:
| Medication Category | Peeing More: % of Users Affected |
|---|---|
| Tamsulosin | 20-30% |
| Diuretics | 70-80% |
| SSRIs/Tricyclic Antidepressants | 10-20% |
| Blood Pressure Meds | 10-15% |
| Antipsychotics | 8-15% |
You might be wondering about tamsulosin and increased urine frequency. For a full rundown—including the science and how UTIs factor in—check out does tamsulosin make you pee more. That post dives into the details, especially for people worried about both peeing more and infections.
Don’t forget—every drug has its own quirks, and your reaction might be totally different from your buddy’s. Sometimes, you have a mix of meds working together, giving your urinary tract double trouble. If you’ve noticed things getting worse since adding or changing a medication, it’s definitely something to bring up with your doctor.

Managing the Side Effects Without Going Nuts
If your bathroom has become your second home, there’s good news: you absolutely can manage these side effects and get some control back. Let’s tackle some real-life fixes—stuff that actually works and isn’t just wishful thinking.
First up, track your pee schedule. It sounds weird, but jotting down when you go (and how much) for a few days gives you and your doctor real info to work with. You’ll start seeing patterns, like “Wow, every time I take my meds at breakfast, I’m in the bathroom nonstop for hours.” Moving the timing of your meds can sometimes help—just don’t make changes without getting your doctor on board first.
If you’re on a diuretic, ask your provider if you can take it earlier in the day. It won’t totally fix things, but at least you might not be wide awake at 2 AM needing to pee. For tamsulosin, sometimes a small shift in when you take it can ease the frequency, though most people get used to the new schedule after a week or two. Other pills, like blood pressure meds, might allow for some flexibility too. The point is, there’s usually some wiggle room.
Hydration gets tricky. Some people try to fix things by barely drinking, but that only backfires. Dehydration makes your urine super concentrated and can irritate your bladder, so you actually end up peeing more often (trust me, it’s a weird irony). Instead, space fluids out during the day, and taper your intake after dinner to avoid midnight bathroom runs. If your meds cause dry mouth on top of everything, suck on ice chips or sugarless hard candy—works surprisingly well to help you feel less parched without guzzling water.
The foods you eat can mess with things too. Salty and spicy meals, artificial sweeteners, carbonated drinks, and caffeine can all irritate your bladder. Nobody says you have to quit coffee for good, but swapping your afternoon latte for herbal tea, or choosing low-salt snacks, can mean fewer urgent dashes. Alcohol is another trigger—so it might make a movie night better, but it can be murder on your bladder if you’re already dealing with side effects.
There’s also muscle training out there for bladders. “Bladder retraining” might sound a bit cheesy, but it’s backed by real evidence. Basically, you hold off on peeing just a little each time, teaching your bladder to cope with more volume without getting twitchy. After a couple weeks, many people can stretch out the time between trips significantly. Pelvic floor exercises, a.k.a. Kegels, are another secret weapon—stronger muscles help your bladder hold on longer, especially after fifty, or for women who’ve had kids.
Worried about leaks? Adult liners are way better than they used to be (not those huge pads from the drugstore aisles of the ‘90s). Some brands are almost invisible and make a hectic day at work way less stressful. If incontinence is getting in the way of daily life, definitely mention it—there’s a surprising amount your provider can do, from meds tweaks to new kinds of therapy.
Try to stay honest with your healthcare team. Embarrassment is normal, but remember—they hear this stuff constantly and will probably be glad you brought it up, instead of guessing why you never sleep or why your routines have changed. Sometimes, a small dose adjustment makes all the difference.
When to Take Action (and When to Worry)
So, you’re tired of running to the toilet, but how do you know if it’s side effects or a bigger health problem? Here’s the real talk: if you just started a new med and notice a change, it’s probably the drug. But there are signs you shouldn’t ignore.
- Your urine’s suddenly cloudy, bloody, or has a weird smell.
- You get pain, burning, or fever along with all the new trips to the bathroom.
- You’re peeing so often you can’t function—like, you can’t sit through a meeting, drive, or sleep for more than an hour at a time.
- You lose control fully or can’t pee at all (yes, it happens—and yes, that’s an emergency).
- The symptoms started way before you began medication, or just keep escalating regardless of meds.
Kidneys are sensitive; ignoring certain symptoms can lead to more than just lost sleep. If in doubt, check in with your doc—if nothing else, you can get reassurance that you’re not making a mountain out of a molehill.
Here’s a tip that surprises most people: sometimes stopping or swapping one of your meds is all it takes. It’s not about “toughing it out.” If you think you’re stuck with these side effects for life, think again. Your team might have a workaround, a different class of drug, or even a non-pill option that works better for you and your bladder.
In rare cases, excess urination can signal medical problems like diabetes, infections, or even heart and kidney issues. That’s why doctors ask so many questions—it’s not just about the inconvenience, but making sure nothing more serious is going on. Bring a list of your meds to every appointment. You’d be shocked how many people forget to mention the over-the-counter stuff, supplements, or herbal teas that are also part of the puzzle.
Let’s face it—nobody dreams about extra bathroom time. But you’re not alone. Medications do all kinds of weird things to your body, and needing to pee more is just one of the common trade-offs. The most important move is to speak up, stay aware of your symptoms, and never accept misery as normal if there might be an easy solution.







17 Comments