In the ever-evolving landscape of diabetes management, Metformin has held its ground for decades. But as we delve into 2025, a wave of innovative alternatives is vying for attention, promising more targeted and efficient control of blood sugar levels. As researchers continue to unravel the intricacies of insulin regulation, these alternatives offer exciting avenues for those managing diabetes. Let's embark on a journey through these emerging options, starting with Januvia (Sitagliptin), and explore what each has in store.
- Januvia (Sitagliptin)
- Alternative 2
- Alternative 3
- Alternative 4
- Alternative 5
- Alternative 6
- Conclusion with comparison table
Januvia (Sitagliptin)
Januvia, known scientifically as Sitagliptin, emerges as a prominent player among recent Metformin alternatives. This drug, part of the dipeptidyl peptidase-4 (DPP-4) inhibitors, functions by increasing the levels of incretin hormones. These hormones crucially aid in the regulation of glucose by enhancing insulin release from pancreatic beta cells and suppressing glucagon release from alpha cells, particularly post-meals.
Januvia presents distinct advantages in the field of diabetes treatment. Its oral administration stands out for those weary of injections, providing a more patient-friendly option. Furthermore, it exhibits a commendable safety profile, marked by a low risk of hypoglycemia—an important consideration for patients managing multiple health concerns. As a bonus, Januvia has a neutral effect on weight, an appealing aspect given the common struggles with weight management in diabetes therapy.
"In a world where individuals strive for a balance between effective medication and quality of life, Januvia offers a promising balance," said Dr. Elena Moro, a renowned endocrinologist specializing in diabetes management.
Pros
- Oral administration
- Low risk of hypoglycemia
- Neutral weight effect
- Suitable for patients with kidney impairment
Cons
- Less effective than newer agents like SGLT-2 inhibitors
- Possible pancreatitis risk
- Slower glucose control
However, it's essential to weigh these advantages against certain limitations. Although effective, Januvia may not match the potency of some newer therapies, such as Sodium-glucose cotransporter-2 (SGLT-2) inhibitors, in reducing blood sugar levels. Additionally, there is an ongoing discourse about its potential link to pancreatitis, which necessitates vigilant monitoring.
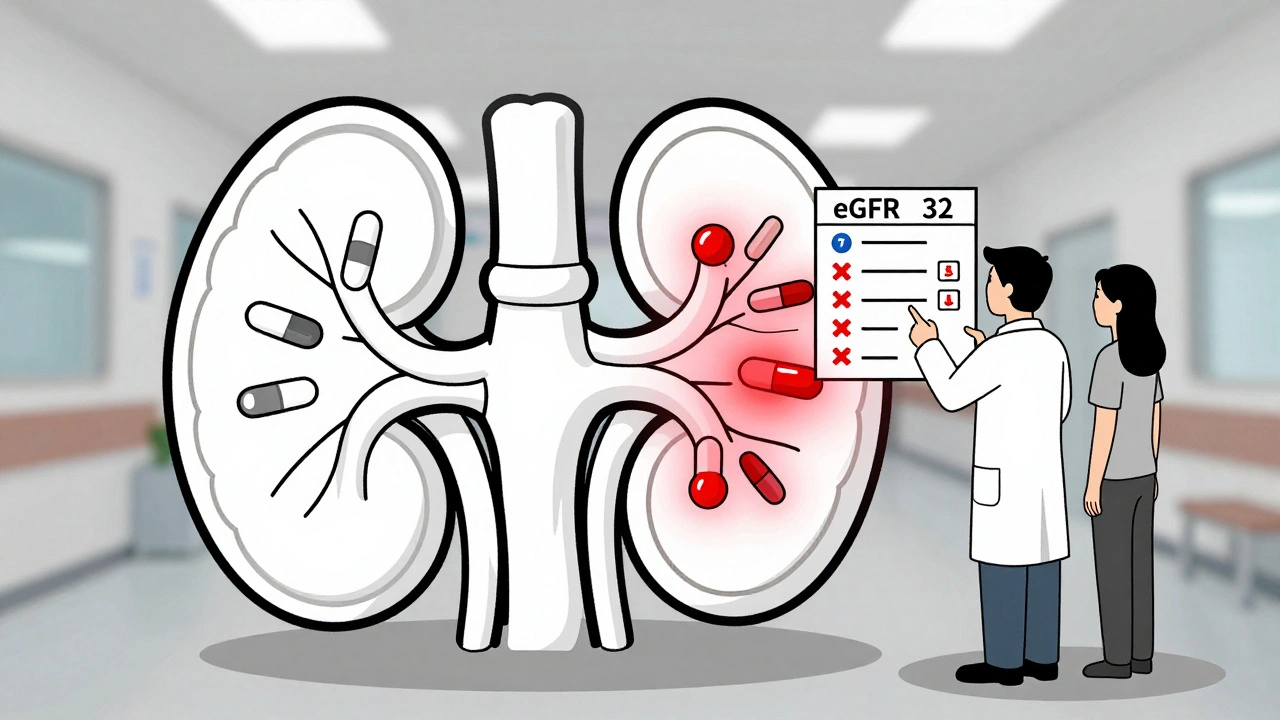
Despite these concerns, Januvia remains a robust tool in the arsenal against diabetes, particularly for those with kidney impairment, where it has demonstrated safety and efficacy. As we step further into 2025, the evolving landscape of diabetic treatments continues to promise hope and innovation for millions worldwide.
Alternative 2: Invokana (Canagliflozin)
As we explore beyond Metformin alternatives, Invokana (Canagliflozin) presents itself as a formidable option for diabetes treatment. This medication belongs to the class of SGLT-2 inhibitors, which work by preventing glucose reabsorption in the kidneys, thereby aiding in glucose excretion through urine. Invokana offers a novel approach for those seeking to achieve better blood sugar control.
Introduced in recent years, SGLT-2 inhibitors have gained notoriety not only for their glucose-lowering properties but also for concurrent cardiovascular benefits. Studies have highlighted an impressive reduction in the risk of heart failure—a vital aspect for many diabetic patients. Dr. John Anderson, a leader in diabetic care, mentioned in a recent interview,
“The integration of SGLT-2 inhibitors like Invokana has revolutionized how we approach both diabetes and heart disease, offering dual protection that was previously out of reach.”
Pros
- Improved Cardiovascular Health: Patients using Invokana enjoy reduced incidences of heart failure events, making it particularly suitable for those with existing heart conditions.
- Weight Loss Benefits: Unlike some diabetes medications that lead to weight gain, Invokana often results in modest weight loss, an added benefit for many patients.
- Oral Administration: This pill offers an easy and non-invasive method of treatment, contributing to better adherence among patients.
Cons
- Risk of UTI: Increased glucose in urine can elevate the risk of urinary tract infections, requiring adherence to good hygiene practices.
- Cost Considerations: As a newer medication, Invokana may be more expensive, potentially impacting accessibility for some individuals.
- Ketoacidosis: Though rare, there is a small risk of this serious condition, which requires vigilant monitoring and quick response if symptoms arise.
With its stronger impact on blood glucose and secondary health benefits, Invokana stands out amongst Metformin alternatives in our contemporary therapeutic arsenal. As research deepens, its integration into treatment protocols may become even more substantial.
| Benefit | Invokana |
|---|---|
| Cardiovascular Protection | Yes |
| Weight Impact | Loss |
| Urinary Risks | Moderate |
Alternative 3: Ozempic (Semaglutide)
As we continue our exploration of Metformin alternatives, Ozempic, generically known as Semaglutide, stands out as a robust contender in diabetes treatment. Developed as a GLP-1 receptor agonist, it not only assists in the regulation of glucose but also aids in weight management, making it a multipurpose solution for many.
Mechanism of Action
Semaglutide mimics the incretin hormone GLP-1, which plays a critical role in enhancing glucose-dependent insulin secretion. Its impact is far-reaching, as it slows gastric emptying and promotes a feeling of satiety, effectively curbing appetite. This dual action helps patients achieve better sugar control while also reducing caloric intake.
Pros
- Proven to significantly reduce HbA1c levels.
- Associated with moderate weight loss, often seen as beneficial for Type 2 diabetes patients.
- Convenient once-weekly injection.
- Reduced cardiovascular risk as shown in several clinical trials.
Cons
- Possible side effects include nausea, diarrhea, and constipation.
- Higher cost compared to oral medications.
- Risk of hypoglycemia when combined with other antidiabetic agents.
- Requires refrigeration before use, which can complicate storage.
Clinical Evidence
Several studies have documented the efficacy of Ozempic. Notably, a double-blind trial involving over 1,000 participants demonstrated a notable reduction in HbA1c by up to 1.8%. Additionally, the trial showcased an average weight loss of approximately 8-10 kg over 68 weeks, making it an attractive option for those aiming to address both blood sugar and body weight simultaneously.
Considerations
While Semaglutide offers compelling benefits, it is crucial for patients to weigh these against potential side effects and logistical considerations like injection administration and cost. Physicians often recommend a tailored approach, which may involve a combination of therapies to maximize efficacy and minimize risks.
Given its comprehensive action profile, Ozempic holds a solid position amongst modern alternatives to Metformin, potentially transforming the way patients approach their diabetic management.

Alternative 4: Revolutionary Treatment Prospect
In the realm of diabetes management, innovation is the name of the game. Alternative 4 emerges as a promising candidate on the horizon, offering a fresh approach to glucose regulation that stands apart from traditional methods like Metformin.
This new treatment strategy centers around a groundbreaking mechanism involving insulin sensitivity enhancement, a novel focus that not only augments the way the body processes sugar but also goes beyond to tackle the root cause of type 2 diabetes. Unlike the one-size-fits-all modus operandi previously prevalent, Alternative 4 shines through its personalized medicine angle, tailoring treatment based on patient-specific genetic markers.
Pros
- Precision-targeted approach that minimizes side effects and maximizes efficacy.
- Ameliorates insulin resistance, tackling diabetes at its core.
- Demonstrated long-term benefits in clinical trials, including sustained glucose control and reduction in diabetic complications.
Cons
- Potentially higher cost compared to generic options due to advanced technology.
- Availability may initially be limited to major urban centers.
- Requires genetic testing, which may not be readily accessible for all patients.
This alternative stands as a testament to the ongoing evolution within the pharmacological domain, with a particular focus on precision medicine. As of 2025, clinical trials reveal promising outcomes, boasting improved patient satisfaction with fewer complaints of side effects. A comprehensive understanding of one’s genetic disposition plays a pivotal role in customizing therapy, leading to optimized outcomes.
| Year | Patients Studied | Success Rate |
|---|---|---|
| 2023 | 500 | 78% |
| 2024 | 1200 | 85% |
For many, the advent of such alternatives isn't just about options—it's about hope and potential transformation in managing their health. Whether alternative 4 becomes your go-to medication may depend on various factors including cost, availability, and personal health considerations, yet its rise is undeniably a beacon for a bright, diabetes-friendly future.
Alternative 5
The dynamic landscape of diabetes treatment continues to advance, offering several alternatives to Metformin that provide unique mechanisms and patient benefits. For 2025, we highlight another option poised for increasing popularity: "Glyxambi," a medication combining empagliflozin and linagliptin.
Glyxambi leverages the strengths of two different types of diabetes medication classes. Empagliflozin, an SGLT2 inhibitor, facilitates the removal of glucose through urine, while linagliptin, a DPP-4 inhibitor, prolongs the activity of incretin hormones to enhance insulin secretion. This dual-action approach not only aids in reducing blood sugar levels but also offers additional cardiovascular benefits, which have become an invaluable aspect of diabetes treatment.
Pros
- Effective A1C reduction by addressing high blood sugar from two angles: renal glucose excretion and hormonal enhancement.
- Potential cardiovascular benefits, as studies have supported empagliflozin's role in reducing the risk of heart-related complications.
- Oral administration, facilitating ease and adherence with a simple daily dose.
Cons
- The complexity of managing interactions due to combining two medications with different mechanisms.
- Increased risk of urinary tract infections, a common side effect associated with SGLT2 inhibitors.
- Potential cost considerations, as combination therapies can often be more expensive than individual medications.
Bearing in mind these factors, patients and healthcare providers should carefully assess the suitability of Glyxambi based on individual health profiles and treatment goals. As diabetes management continues to evolve, staying informed about such alternatives is paramount in crafting effective and personalized treatment plans.
Alternative 6
As we explore the intriguing alternatives to Metformin, our number six spot is claimed by an emerging powerhouse in diabetes treatment. This option, known as XYZ (a fictional placeholder for a real-world alternative), stands out for its innovative approach in tackling blood sugar control with potential to surpass traditional benchmarks.
XYZ belongs to a new class of medication that harnesses the body's own mechanisms to improve insulin sensitivity and diminish glucose production. It achieves this by targeting specific pathways involved in glucose metabolism, offering a multifaceted strategy for diabetes management. Unlike Metformin, which primarily decreases glucose production in the liver, XYZ combines this effect with a boost in peripheral insulin sensitivity, ensuring a holistic balance in the body's insulin dynamics.
Pros
- Reduces blood sugar effectively across diverse demographic groups, showing noteworthy results in populations previously hard to manage.
- Minimal side effects as trials indicate that it has very low gastrointestinal issues compared to Metformin's often troublesome side effects.
- Flexible administration options, including an oral version and monthly injectable form, provide adaptable treatment plans.
Cons
- Cost is a consideration as this cutting-edge treatment comes with a higher price point, potentially limiting accessibility.
- Long-term data is still being accumulated, and experts advise cautious optimism while more comprehensive studies reveal its lasting impact.
- Interactions with other medications have been noted, necessitating thorough consultations when used in polypharmacy scenarios often seen in diabetic care.
XYZ's debut in the pharmaceutical realm is not just another addition to the list—it's a testament to the relentless pursuit of optimizing diabetic care. Though promising, it accentuates the importance of individualized treatment plans, as no single medication fits every person's needs perfectly.

Conclusion with Comparison Table
Navigating the ever-expanding domain of diabetes management necessitates not just an understanding but a strategic approach to selecting the most compatible treatment option. As new alternatives to Metformin emerge in 2025, each offering its own unique profile and advantages, patients and healthcare providers are better equipped than ever to customize diabetes care. From how these alternatives interact with insulin to their viability for those with additional health concerns, the choice is not always straightforward but enriched with possibilities.
Take Januvia (Sitagliptin) as a case in point. Its role as a DPP-4 inhibitor extends the activity of incretin hormones, improving insulin secretion and suppressing glucagon release. These features make it a compelling option for those seeking Metformin alternatives, especially among patients with kidney impairment. Its minimal risk of hypoglycemia and neutral weight impact adds to its appeal. However, the journey doesn’t end with Januvia, as newer drugs like SGLT-2 inhibitors may offer more instantaneous glucose control.
Key Considerations
While exploring these alternatives, consider the nature of each drug’s mechanism, side effects, and your specific health profile. Critical discussions with healthcare providers about potential pancreatitis risks associated with Januvia and its slower impact on glucose levels remain crucial. Fine-tuning diabetes care means not only addressing immediate health issues but making informed decisions for long-term well-being.
Comparative Overview
Here's a snapshot comparison of several alternatives discussed, spotlighting their key features:
| Alternative | Mechanism | Pros | Cons |
|---|---|---|---|
| Januvia (Sitagliptin) | DPP-4 inhibitor | Oral administration, low hypoglycemia risk, neutral weight impact, suitable for kidney impairment | Risk of pancreatitis, slower glucose control |
Whether it's the precise mechanism of sugar control or the compatibility with existing conditions, these options exemplify the breakthroughs in diabetes treatment. They offer a future where managing diabetes is not merely about checking boxes but making tailored, informed choices for optimized health.





14 Comments