Every year, thousands of people in the U.S. and Australia get the wrong medication-not because of a mistake in dosage, but because two drug names look or sound almost identical. Look-alike and sound-alike (LASA) drug names are one of the most dangerous but overlooked risks in healthcare. You might think pharmacists and nurses would catch these errors, but the truth is, even trained professionals miss them-especially under time pressure. The good news? There are clear, proven ways to spot these dangerous mix-ups before they happen.
What Makes Two Drug Names Look or Sound the Same?
It’s not just about spelling. Two drugs can be dangerously similar if they share 60-80% of their letters. For example:
- HydroXYZINE (for anxiety) vs. HydroALAZINE (for high blood pressure)
- DoXEPamine (for depression) vs. DoBUTamine (for heart failure)
- CISplatin (for cancer) vs. CARBOplatin (also for cancer)
These aren’t typos. They’re approved names that were never designed with safety in mind. A 2023 FDA report found over 3,000 such pairs in use. The problem gets worse when prescriptions are handwritten or printed on low-quality labels. In fact, nearly 41% of LASA errors come from illegible handwriting, and 29% from faded or poorly printed labels.
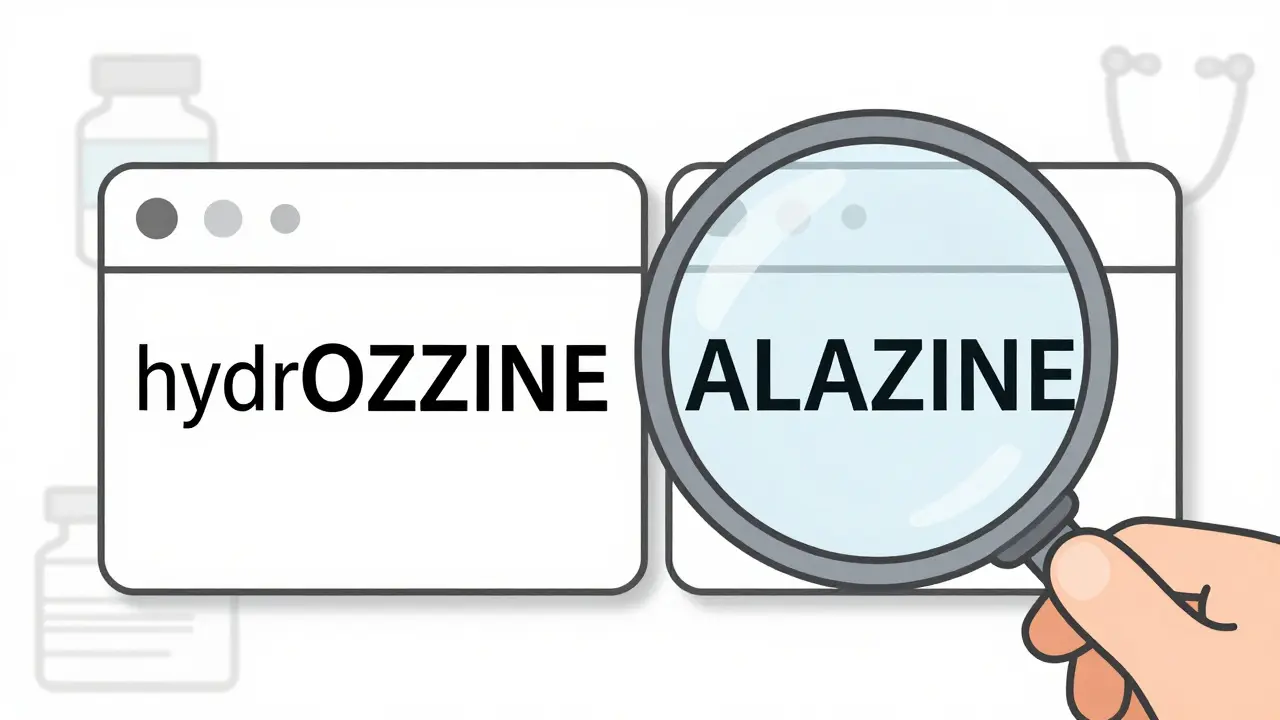
Tall Man Lettering: The Visual Clue You Need to Know
The most effective tool to catch these errors is called tall man lettering. It’s a simple trick: capitalize the letters that make two similar names different. Instead of writing hydroxyzine and hydroalazine, you write hydrOXYZINE and hydrALAZINE.
This isn’t just a suggestion-it’s a standard. The FDA has officially recommended tall man lettering for 35 high-risk drug pairs as of 2024. Hospitals, pharmacies, and electronic health systems are required to use it. Look for these capital letters on:
- Pharmacy labels
- Electronic prescribing screens
- Automated dispensing cabinets (like Pyxis machines)
- Medication administration records (MARs)
Studies show tall man lettering alone cuts visual confusion errors by 32%. But here’s the catch: it only works if it’s used consistently. One nurse in Sydney reported that her hospital’s EHR system showed tall man letters for hydroCODONE, but the printed MAR didn’t. She almost gave the wrong drug because of the mismatch.
Don’t Rely on Visuals Alone
Tall man lettering helps-but it’s not foolproof. A 2022 study in the Journal of Patient Safety found that combining tall man lettering with color coding and purpose-of-treatment notes increased error prevention to 59%. That means:
- Color: High-risk drugs like insulin or anticoagulants might have a red or yellow background on labels.
- Text: The label should say why the drug is being given-e.g., “for atrial fibrillation” next to warFARIN or “for seizure control” next to LEVETIRACETAM.
These extra details force you to think, not just recognize. If you see a drug labeled “for pain” and it’s oxycodONE, you know it’s not oxycodIN (a different drug). Purpose-of-treatment info reduces errors by 27% more than tall man lettering alone.

How to Protect Yourself or a Loved One
You don’t need to be a pharmacist to spot a dangerous mix-up. Here’s what you can do:
- Read the full label every time. Don’t just glance at the first few letters. Look for capitalized letters that stand out.
- Ask: “What is this for?” If the label doesn’t say, ask the pharmacist. A drug named valCYclavir and valACYclovir might look similar, but one treats cytomegalovirus, the other herpes. If you’re not sure why it’s prescribed, dig deeper.
- Compare the name to your previous prescription. If your last refill was metFORMIN and now it’s metGLIPIZIDE, that’s a big change. Don’t assume it’s the same.
- Check the bottle shape and color. Even if the name looks right, if the pill looks different from before, ask about it.
- Use barcode scanning if available. Many hospitals now scan medications at every step-from pharmacy to bedside. If you’re in a hospital, ask if they scan before giving you a drug.
A 2021 study at UCSF found that pharmacists who spent just 2-3 minutes double-checking high-risk pairs reduced errors from 18% to just 3%. That’s a 83% drop. You can do the same.
Why Computer Systems Sometimes Fail You
Electronic systems are supposed to help-but they can also cause problems. Many EHRs show too many drug options when you type in just two or three letters. If you type “oxy,” you might see 15 different drugs. That’s a recipe for clicking the wrong one.
Best practice? Systems should require at least five letters before showing results. That cuts down confusing lists by 68%. Also, confusing pairs like hydralAZINE and hydroXYZINE should never appear next to each other in dropdown menus. The Office of the National Coordinator for Health IT made this a requirement in 2019. If you see them side-by-side, it’s a red flag.
And then there’s alert fatigue. When a system pops up a warning for every possible mix-up-even low-risk ones-clinicians start ignoring them. A 2021 JAMA study found that nearly half of all LASA alerts are overridden. The fix? Alerts should only trigger for the FDA’s top 35 high-risk pairs.

What’s Changing in 2025 and Beyond
Things are getting better-but slowly. In 2023, the FDA added 12 new drug pairs to its tall man lettering list, bringing the total to 35. By December 2024, all U.S. and Australian healthcare systems must implement these changes. The National Council for Prescription Drug Programs also rolled out a new data standard in early 2023 that lets systems share LASA warnings in real time across pharmacies, hospitals, and insurers.
AI is stepping in too. Google Health’s Med-PaLM 2 can now predict which drug names might cause confusion with 89% accuracy. But it’s not replacing humans-it’s helping them. The goal isn’t to automate safety. It’s to make humans better at it.
One hospital in Baltimore cut LASA errors by 67% over two years by combining tall man lettering, mandatory purpose notes, and staff training. That’s the model. No single fix works alone. It’s the combo that saves lives.
Final Checklist: Five Questions to Ask Before Taking Any Prescription
Before you leave the pharmacy or take a pill at home, ask yourself:
- Is tall man lettering used? Are there capital letters in the middle of the name?
- Does the label say why I’m taking this drug?
- Does the pill look like the one I took last time?
- Did the pharmacist confirm this is the right drug for my condition?
- If I’m unsure, can I call the pharmacy back before taking it?
If you answer “no” to any of these, stop. Ask again. You’re not being difficult-you’re being smart.
What are the most common look-alike drug name pairs I should watch for?
The FDA’s top 35 high-risk pairs include: hydrOXYZINE vs. hydrALAZINE, doXEPamine vs. doBUTamine, CISplatin vs. CARBOplatin, metFORMIN vs. metGLIPIZIDE, and hydralAZINE vs. hydroXYZINE. These are the names that cause the most mix-ups. Always check for capitalized letters in the middle of the word-those are the key differences.
Is tall man lettering used in Australia?
Yes. Australia follows international safety standards, and most public and private hospitals use tall man lettering for high-risk drugs. The TGA (Therapeutic Goods Administration) recommends it, and many EHR systems in Australia now include it by default. However, private pharmacies and handwritten prescriptions may still lack it, so always double-check.
Can I trust the name on the label if it’s printed by a pharmacy?
Not always. Low-quality printers, faded ink, or small fonts can make tall man lettering hard to read. If the capital letters look smudged or too small to distinguish, ask for a new label. The Joint Commission requires labels to be printed in at least 12-point font with a 4.5:1 contrast ratio. If it’s hard to read, it’s not safe.
Why do some prescriptions still have errors even with tall man lettering?
Because safety isn’t just about labels. Time pressure, distractions, poor training, and inconsistent systems all play a role. One nurse might see tall man letters on the screen, but the printed label doesn’t have them. Or a doctor writes a prescription by hand without using it. Technology helps-but human vigilance is still the last line of defense.
What should I do if I think I got the wrong medication?
Don’t take it. Call your pharmacist or doctor immediately. Bring the label and the pill bottle with you. Report the incident-even if you didn’t take the drug. These near-misses help improve safety systems. The ISMP receives over 4,700 LASA error reports annually, and each one helps prevent future mistakes.
Next Steps for Safer Medication Use
If you’re a patient: Always read the label. Ask about the purpose of the drug. Keep a list of your medications and their exact names.
If you’re a caregiver: Double-check every prescription. Don’t assume the pharmacist got it right. Use the five-question checklist before handing over a pill.
If you work in healthcare: Push for consistent tall man lettering across all systems. Advocate for purpose-of-treatment notes. Push back on alert fatigue by demanding smarter, targeted warnings.
Medication safety isn’t about perfection. It’s about layers. Tall man lettering is one layer. Purpose notes are another. Your vigilance is the most important one of all.







10 Comments