It starts with a red, itchy rash-maybe on your wrists, neck, or hands. You didn’t touch anything unusual. No new soap, no new jewelry. But the rash won’t go away. It flares up every few days, then fades, only to return again. You’ve tried hydrocortisone, moisturizers, even switching to "hypoallergenic" products. Nothing works. If this sounds familiar, you might have contact dermatitis-specifically, allergic contact dermatitis (ACD). It’s not just dry skin. It’s your immune system reacting to something you’re touching every day.
What’s Actually Causing Your Rash?
Unlike immediate allergic reactions like peanut or bee sting allergies, contact dermatitis is a slow burn. It takes 24 to 72 hours for your skin to react after touching the trigger. That’s why it’s so hard to connect the dots. You might think your new shampoo caused the rash, but it could be the nickel in your jeans button, the fragrance in your laundry detergent, or even the preservative in your hand cream.
The real culprit? Low-weight chemicals called haptens. These tiny molecules sneak past your skin’s barrier, latch onto your skin proteins, and trick your immune system into thinking they’re invaders. Your body sends out T-cells to fight them-and that’s what causes the redness, swelling, and itching. Over 3,000 substances can trigger this reaction, but only a handful show up again and again.
Nickel is the biggest offender. It’s in jewelry, belt buckles, zippers, phone cases, and even some eyeglass frames. Studies show 17.4% of women and 3% of men in North America are allergic to it. That’s one in five women. And it’s not just jewelry-nickel leaches from stainless steel cookware, tools, and even coins. In Europe, laws limiting nickel in jewelry cut allergy rates by 25% since 2004. But in the U.S., there’s no such rule.
How Do You Know What’s Triggering It?
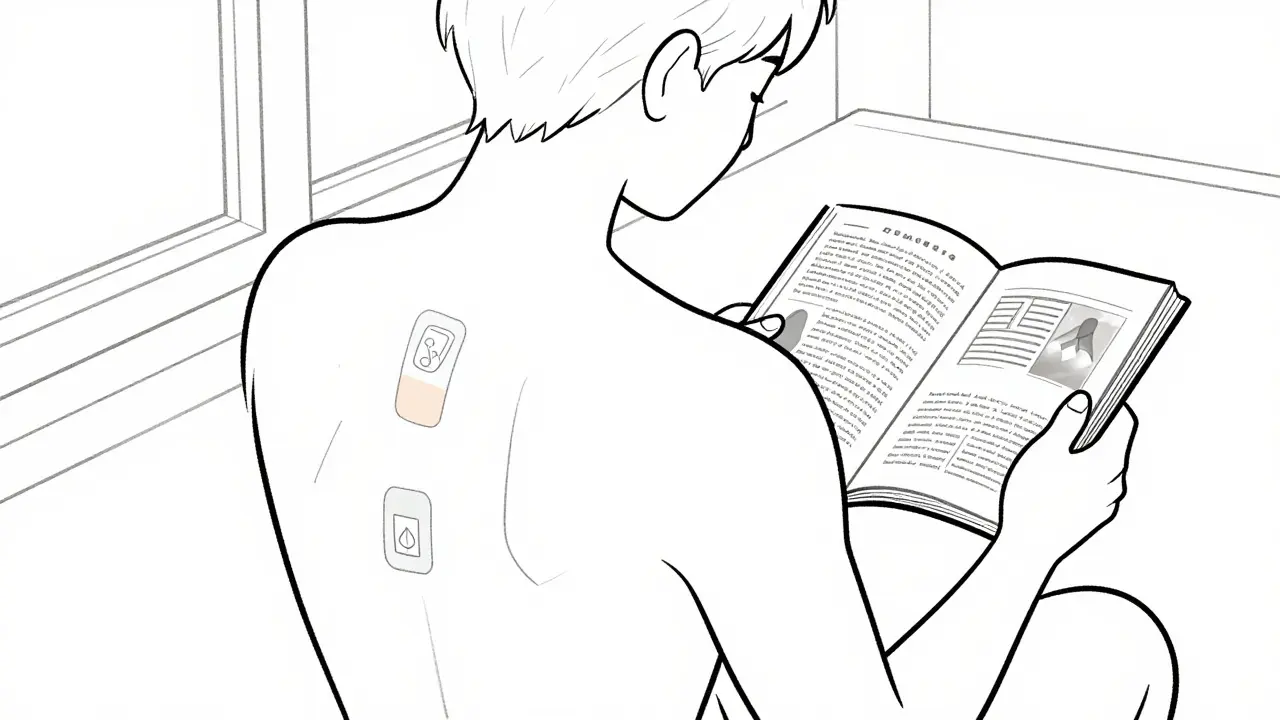
Guessing won’t cut it. The only reliable way to find your trigger is through patch testing. It’s not a needle. It’s not a blood test. It’s small patches glued to your back, each containing a tiny amount of a common allergen. You wear them for 48 hours, then return for the first reading. You come back again at 96 hours for the final check. That’s it.
The standard test, called the TRUE Test, checks for 29 common allergens. The top five? Nickel sulfate (found in 14.7% of positive tests), thimerosal (a preservative in some eye drops), cobalt chloride (in metal alloys and paints), fragrance mix (a blend of 8 common scents), and balsam of Peru (used in cosmetics, perfumes, and even some foods like cinnamon and vanilla).
But here’s the catch: 29 allergens isn’t enough. Many people test negative on the standard panel, then find their trigger with expanded testing-up to 70 or even 100 allergens. A 2023 study found 33% of patients needed extra testing to find their cause. One Reddit user, after five years of rashes, finally found out they were allergic to cocamidopropyl betaine-a foaming agent in shampoos and body washes. Once they stopped using it, their skin cleared up completely.
Some allergens hide in plain sight. Formaldehyde, for example, is in nail polish, hair straighteners, and even some baby wipes. It’s not listed as "formaldehyde"-it’s often hidden as "quaternium-15," "DMDM hydantoin," or "bronopol." If you’re allergic to formaldehyde, you’ll need a more detailed patch test than the standard panel offers.
What Happens After the Test?
Getting a positive result isn’t the end-it’s the beginning. The real work starts now: avoidance. And it’s harder than it sounds.
Imagine you’re allergic to nickel. You throw out your jewelry. But what about your laptop? Your bra clasp? Your keys? Your watch? You start reading labels. You switch to ceramic or titanium jewelry. You use clear nail polish on the backs of buttons to block nickel leaching. You buy plastic phone cases instead of metal ones. You even start checking the metal parts of your kitchen utensils.
That’s where the Contact Allergen Management Program (CAMP) comes in. Developed by the American Contact Dermatitis Society, CAMP gives you a personalized list of safe products based on your test results. It’s not just a list of ingredients-it’s a list of actual brands and products you can buy. In 2022, their data showed a 78% improvement rate in chronic cases when patients followed CAMP’s recommendations.
The Contact Allergen Replacement Database (CARD) is even more powerful. It’s a living database with over 18,000 consumer products labeled as safe for 27 common allergens. Want to know which moisturizer doesn’t contain fragrance mix? Which sunscreen avoids balsam of Peru? CARD tells you. And it’s updated regularly-new products added every month.
Why Some People Still Struggle
Even with a clear diagnosis, avoidance isn’t always easy. Many patients report frustration with hidden allergens. One woman found her rash cleared up after switching shampoos-but then returned after three weeks. She hadn’t realized her new conditioner had the same preservative. Another man thought he was allergic to latex gloves at work, but his patch test showed he was reacting to the powder inside the gloves, not the latex itself.
And it’s not just consumer products. Occupational exposure is a huge factor. Hairdressers have a 42% allergy rate-mostly to paraphenylenediamine (PPD) in hair dye. Nurses and doctors often react to chlorhexidine in antiseptic wipes or neomycin in topical creams. Construction workers deal with chromates in cement. If you work in one of these fields, your employer should help identify and reduce exposure. OSHA guidelines require it.
Even then, some allergens are impossible to avoid completely. Fragrance is in everything: soap, lotion, laundry detergent, air fresheners, even some medications. The EU restricts 26 fragrance allergens in cosmetics. The U.S. doesn’t. That’s why fragrance allergy affects 1-4% of the population-and why many people need expanded patch testing to find the exact scent causing their flare-ups.
What’s Changing in Diagnosis and Treatment
Things are getting better. In 2025, the American Contact Dermatitis Society is launching an expanded TRUE Test with 80 allergens, including newer triggers like those found in green cosmetics and smartphone components. Researchers are also exploring blood tests that measure IL-18 levels, a protein that spikes during active contact dermatitis. Early results show it correlates strongly with rash severity.
Animal testing for allergens is being phased out. The EU will ban guinea pig tests by 2027. New methods, like computer modeling and cell-based assays, are replacing them. But here’s the truth: nothing beats patch testing yet. Dr. Howard Maibach, a leading dermatologist, says it best: "Patch testing remains irreplaceable for clinical diagnosis. Molecular methods help, but they’re still assistants-not replacements."
For now, the best advice is simple: if you’ve had a persistent rash for more than a few weeks, get tested. Don’t wait. Don’t keep guessing. Don’t assume it’s just "dry skin."
What You Can Do Right Now
You don’t need to wait for a doctor’s appointment to start making changes.
- Stop using all scented products for two weeks-soaps, lotions, detergents, body sprays. Switch to fragrance-free versions.
- Wear white cotton gloves when doing dishes or cleaning. Rubber gloves can contain chemicals that trigger reactions.
- Check your jewelry. If it’s not labeled "nickel-free," avoid it. Use clear nail polish on the backs of buttons and zippers.
- Write down everything you touch daily-your phone, your watch, your wallet, your desk chair. Note when rashes flare.
- Call your dermatologist and ask: "Can I get patch testing?" If they say no, ask for a referral to a contact dermatitis specialist.
It’s not about being perfect. It’s about being aware. One woman in Sydney, after years of rashes, found her trigger was the metal in her yoga mat strap. Once she switched to a fabric strap, her skin cleared up in three weeks. She didn’t need expensive creams. She didn’t need steroids. She just needed to know what she was touching.

How Long Until You See Results?
Most people start to see improvement within two to four weeks of avoiding their trigger. A 2023 survey of 1,247 patients found 82% had significant improvement after avoiding their allergens. But it takes patience. Your skin doesn’t heal overnight. The inflammation has to calm down. The immune cells have to stop reacting.
Some people need to avoid their trigger for months before their skin fully recovers. That’s normal. The key is consistency. One slip-up-a new pair of earrings, a new hand soap-can set you back weeks.
When to See a Specialist
See a dermatologist if:
- Your rash lasts longer than two weeks
- It keeps coming back after treatment
- It spreads beyond the area you touched
- You’re using steroid creams more than twice a week
- You’ve tried multiple products and nothing works
A specialist can order patch testing and help you interpret the results. General practitioners often miss contact dermatitis because it looks like eczema or psoriasis. But the treatment is completely different.
Can contact dermatitis go away on its own?
Yes, if you stop touching the allergen. But if you keep exposing your skin to the trigger, the rash will keep coming back. The immune system remembers the allergen, so even years later, a small touch can cause a flare-up. Avoidance is the only cure.
Is patch testing painful?
No. The patches are taped to your back and don’t hurt. You might feel slight itching or irritation where the allergen is reacting, but that’s part of the diagnosis. There are no needles, no blood draws. It’s non-invasive and safe.
Can I do patch testing at home?
No. Patch testing requires medical supervision. Applying allergens incorrectly can cause burns, false positives, or missed diagnoses. Only trained dermatologists or allergists should perform it. DIY tests online are unreliable and can make things worse.
Are natural products safer?
Not necessarily. Many "natural" products contain plant extracts like tea tree oil, lavender, or chamomile-which are common allergens. Essential oils are concentrated and can trigger reactions just like synthetic fragrances. "Natural" doesn’t mean hypoallergenic.
Can I still use makeup if I have contact dermatitis?
Yes, but you need to be selective. Look for products labeled "fragrance-free," "hypoallergenic," and "dermatologist-tested." Avoid anything with "parfum," "essential oils," or "botanical extracts" unless you’ve tested them. The CARD database lists safe makeup brands for common allergens like nickel, cobalt, and preservatives.
Final Thought
Your skin is talking to you. It’s not being dramatic. It’s not just sensitive. It’s telling you something your body can’t ignore. Contact dermatitis isn’t rare. It’s common. And it’s fixable-if you know what you’re dealing with. You don’t need to live with itchy skin forever. You just need to know what’s touching your skin-and then stop it.








8 Comments