When opioids and benzodiazepines are taken together, they don’t just add up-they multiply. This isn’t a mild side effect or a minor concern. It’s a life-threatening combo that can stop your breathing before you even realize something’s wrong. You might be on an opioid for chronic pain and a benzodiazepine for anxiety or insomnia. But if you’re taking both, you’re already at a higher risk than you think. And it’s not just about feeling drowsy. It’s about your body losing the ability to keep you alive.
Why This Combo Kills
Both opioids and benzodiazepines slow down your central nervous system. Opioids act on mu-opioid receptors in the brainstem, the part that controls automatic breathing. Benzodiazepines boost GABA, a calming neurotransmitter that also suppresses the brain’s drive to breathe. Alone, each drug can cause breathing to slow. Together, they don’t just add their effects-they team up in a way that makes your breathing dangerously shallow or even stop entirely. Studies show that people taking both drugs have a 10 times higher risk of dying from an overdose than those taking opioids alone. In 2020, about 16% of opioid-related overdose deaths in the U.S. involved benzodiazepines. That’s not a small number-it’s over 35,000 lives lost in a single year because of this interaction. The CDC found that the rate of deaths from this combo jumped from 0.6 per 100,000 people in 1999 to nearly 9 per 100,000 in 2017. Even though it’s slightly dropped since then, it’s still far too high. One chilling detail: patients who’ve been on opioids for years and think they’ve built up a tolerance aren’t protected. Their bodies may handle the opioid, but they don’t develop tolerance to the respiratory effects of benzodiazepines. That means someone who’s been taking oxycodone for years could still die from a low dose of alprazolam if they start taking it on top of their regular opioid.How It Happens: The Science Behind the Danger
It’s not just about sedation. The real danger is what happens to your airway and oxygen levels. Both drugs cause your upper airway muscles to relax too much. That leads to obstructive sleep apnea-even if you’re awake. Your tongue or throat tissues collapse, blocking airflow. Your brain knows you need oxygen, but the drugs are silencing the signal to breathe harder. Add to that the fact that some opioids (like fentanyl, methadone, and oxycodone) are broken down by an enzyme called CYP3A4. Some benzodiazepines, like alprazolam, block this enzyme. That means your body can’t clear the opioid as fast. Your opioid levels rise, your breathing slows even more, and you’re at risk of overdose even if you’re taking what your doctor called a "normal" dose. A study published in the Annals of Palliative Medicine found that when people took both drugs, 85% of them dropped below 90% oxygen saturation. That’s dangerously low. When they took opioids alone, only 45% did. And in real-world cases, people have gone into respiratory arrest at doses that were perfectly safe when taken separately.Who’s at Risk-and Why Doctors Still Prescribe This
You might assume this is only a problem for people abusing drugs. But it’s not. A 2021 study in JAMA Network Open found that nearly 15% of Medicare Part D patients on long-term opioids were also prescribed benzodiazepines. That’s millions of older adults, many of whom were prescribed these drugs for separate conditions: pain and anxiety, or pain and insomnia. Doctors aren’t always ignoring the risks. Sometimes, they’re desperate. A patient with severe chronic pain and debilitating anxiety might not respond to any other treatment. But the FDA says this combo should only be used when no other options exist. Even then, they recommend starting with the lowest possible dose of the benzodiazepine, not the standard one. And they require close monitoring-something that’s hard to do outside a hospital. The American Geriatrics Society lists this combination as "potentially inappropriate" for older adults. Why? Because older people already have slower metabolism, weaker respiratory muscles, and higher risk of falls. Add this combo, and the chance of a fatal overdose or a broken hip from a fall skyrockets.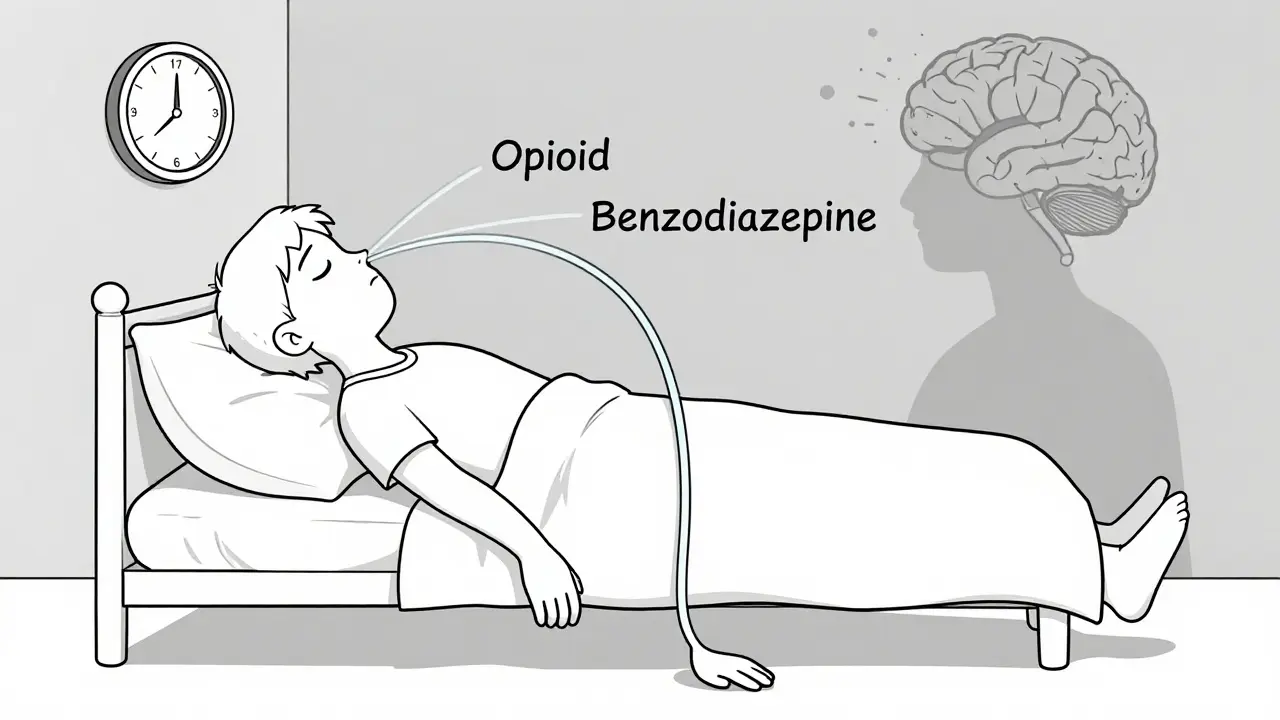
What to Watch For: Signs of Overdose
You don’t need to wait for someone to pass out. The early warning signs are subtle but unmistakable:- Extreme drowsiness-even if they just woke up
- Slow, shallow, or irregular breathing
- Confusion, slurred speech, or difficulty staying awake
- Dizziness or unresponsiveness to stimuli
- Lips or fingertips turning blue
What to Do If You’re Already on Both
If you’re currently taking opioids and benzodiazepines together, don’t stop suddenly. Abrupt withdrawal from either can be deadly. Opioid withdrawal causes intense flu-like symptoms, anxiety, and rapid heart rate. Benzodiazepine withdrawal can trigger seizures, hallucinations, or even death. The right path is a slow, supervised taper. Work with your doctor to reduce one drug at a time. Most experts recommend lowering the benzodiazepine first, since it’s the bigger contributor to respiratory risk. But this must be done carefully-too fast, and you risk seizures or rebound anxiety that leads to relapse. Your doctor should also check:- Which opioid you’re on (fentanyl, methadone, and oxycodone are higher risk)
- Which benzodiazepine (long-acting ones like clonazepam build up in your system)
- Your liver and kidney function (slower clearance = higher risk)
- Whether you drink alcohol or use other sedatives

What’s Being Done to Fix This
The FDA now requires a "Boxed Warning"-the strongest safety alert-on both opioid and benzodiazepine labels, clearly stating the risk of death when combined. Electronic health records now have alerts that pop up when a doctor tries to prescribe both. One study showed these alerts cut inappropriate co-prescribing by over 27%. The CDC has funded research specifically to understand why this combo is so deadly and how to prevent it. Some hospitals now use risk assessment tools to identify patients who are most vulnerable-like those with sleep apnea, COPD, or obesity-before prescribing either drug. And there’s hope on the horizon. New pain treatments are being developed that don’t affect breathing. Non-opioid pain options like gabapentinoids, physical therapy, and nerve blocks are gaining more support. For anxiety, therapies like CBT and non-sedating antidepressants are replacing benzodiazepines as first-line treatment.What You Can Do Right Now
If you’re on either drug:- Ask your doctor: "Is it absolutely necessary to take both?"
- Ask: "Are there safer alternatives?"
- Ask: "What should I do if I feel too sleepy or can’t breathe normally?"
- Make sure someone in your home knows the signs of overdose and has access to naloxone.
- Never mix these drugs with alcohol, sleeping pills, or muscle relaxants.
Can naloxone reverse an overdose from opioids and benzodiazepines together?
Naloxone can reverse the opioid part of the overdose, but it does nothing for the benzodiazepine. That means even if naloxone brings someone back to consciousness, they can still stop breathing because the benzodiazepine is still suppressing their respiratory drive. Emergency medical help is always needed.
Are there any safe doses of this combination?
There is no safe dose when these drugs are combined. Even low doses can be deadly, especially in people with sleep apnea, COPD, or older adults. The FDA and CDC recommend avoiding this combination entirely unless no other options exist-and even then, only with extreme caution, lower doses, and close monitoring.
Why do doctors still prescribe both if it’s so dangerous?
Some doctors prescribe both because they’re treating two separate conditions-pain and anxiety, for example-and don’t realize how dangerous the interaction is. Others feel pressured by patients who say they need the benzodiazepine to sleep or manage anxiety. But guidelines from the FDA, CDC, and American Geriatrics Society now clearly say this combination should be avoided. Better alternatives exist for both conditions.
Can I switch from benzodiazepines to something safer?
Yes. For anxiety, antidepressants like SSRIs (e.g., sertraline or escitalopram) are first-line treatments and don’t cause respiratory depression. For insomnia, cognitive behavioral therapy (CBT-I) is more effective long-term than sleeping pills. These options require time and support, but they’re much safer than benzodiazepines-especially if you’re on opioids.
What if I’ve been on both for years? Can I just stop?
No. Stopping either drug suddenly can be life-threatening. Opioid withdrawal is extremely uncomfortable and can lead to relapse. Benzodiazepine withdrawal can cause seizures, heart rhythm problems, or psychosis. Always work with a doctor to create a slow, supervised tapering plan. Never try to quit on your own.