When pancreatic cancer shows up, it’s often already far along. That’s why so many people are diagnosed too late. The pancreas hides behind the stomach, quiet and out of sight. By the time pain, weight loss, or yellow skin appear, the cancer may have spread. But things are changing. New research is uncovering earlier warning signs, and treatments are getting better - not just for the few who catch it early, but for many more.
What Are the Real Early Signs?
Most people don’t feel sick until the cancer is advanced. But some symptoms show up months before diagnosis - if you know what to look for. The biggest red flags aren’t the ones you’d expect.
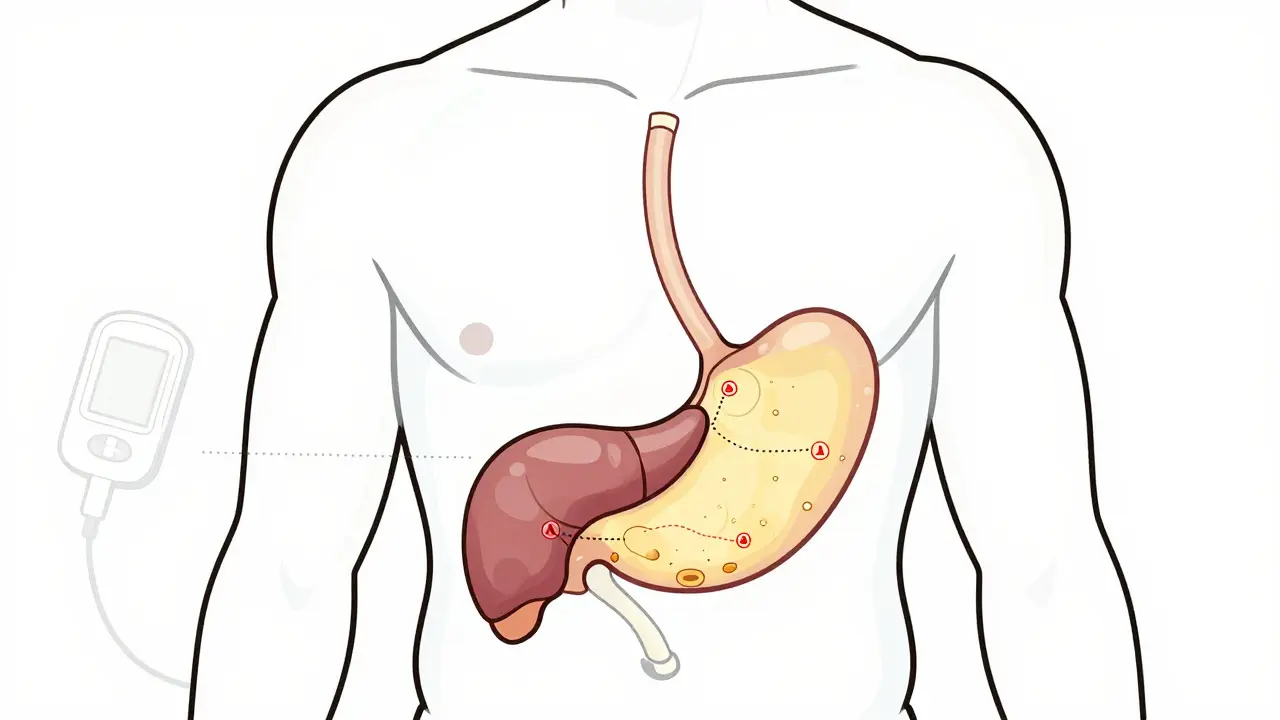
Unexplained weight loss is one of the most common. People lose 10% or more of their body weight without trying. No diet, no exercise - just slipping away. This happens in about 60% of cases, according to the Journal of Clinical Oncology. It’s not just hunger. The pancreas stops making the right enzymes to digest food. Fat passes through undigested, leading to greasy, floating stools. That’s not normal.
Then there’s jaundice. Yellow eyes, dark urine, pale stools. This happens when a tumor in the head of the pancreas blocks the bile duct. Bilirubin builds up in the blood. Levels above 2.5 mg/dL trigger the color change. And it’s not just skin deep - 60% of people with jaundice from pancreatic cancer also have intense itching. It’s not a rash. It’s your body reacting to bile salts stuck in the skin.
New-onset diabetes is another silent signal. If you’re over 50, never had diabetes before, and suddenly your blood sugar spikes - get checked. A 2022 Nature Genetics study found that 80% of pancreatic cancer patients developed diabetes within 18 months of diagnosis. Fasting glucose jumps from normal (under 100 mg/dL) to diabetic levels (over 126 mg/dL) in just six months. This isn’t lifestyle-related diabetes. It’s the tumor messing with insulin production.
Back pain is common too. Not from lifting something heavy. This pain is deep, constant, and gets worse after eating. It radiates from the upper abdomen to the back. About two-thirds of patients report it. Doctors often mistake it for a slipped disc or muscle strain.
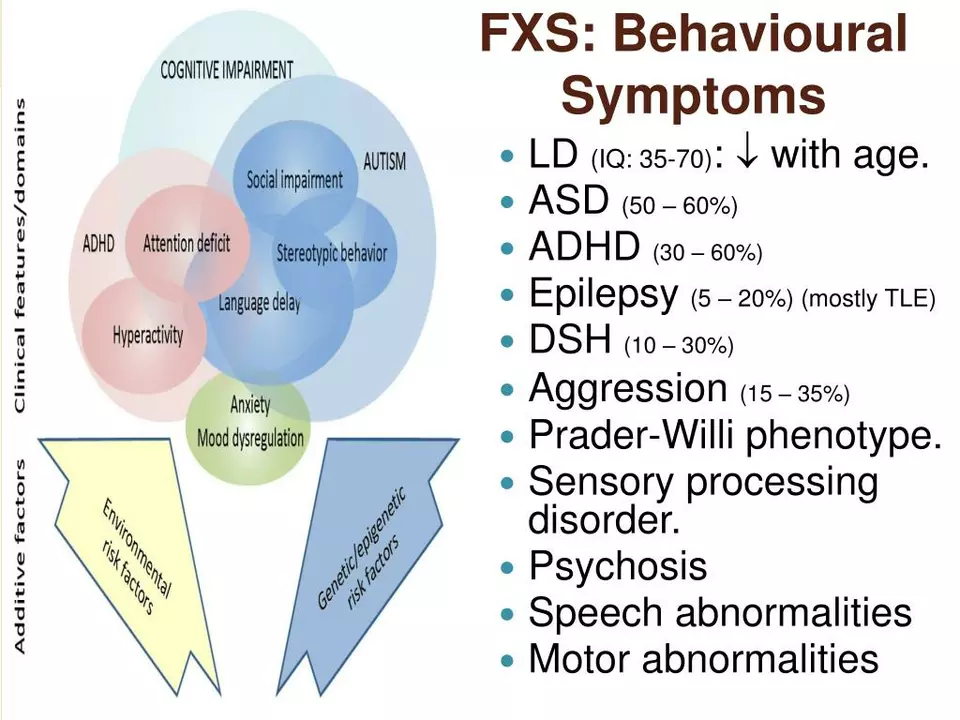
And then there’s the emotional clue - depression. A 2018 study showed that nearly half of pancreatic cancer patients had major depression or anxiety before physical symptoms. For some, it was the first sign. They felt hopeless, tired, unmotivated - and didn’t know why. It’s not just stress. The tumor releases chemicals that affect brain chemistry.
Why Is It So Hard to Catch Early?
The pancreas is tucked behind the stomach, pressed against the spine. No one can feel a tumor there during a physical exam. Blood tests like CA 19-9 aren’t reliable until the cancer is advanced. They miss early tumors up to 70% of the time. Imaging like CT scans only catch tumors larger than 3 cm. Smaller ones? Invisible.
There’s no routine screening for the general public. Unlike mammograms or colonoscopies, there’s no simple test you can get yearly. That’s why most cases - 80% - are found at stage III or IV. By then, surgery is often no longer an option.
But high-risk groups can be monitored. If you have a family history of pancreatic cancer, or carry a BRCA2 mutation, or have hereditary pancreatitis, you may qualify for surveillance. Programs at places like Johns Hopkins use annual MRI and endoscopic ultrasound to catch tumors before they spread. These tests aren’t perfect, but they save lives when used correctly.
What’s Changed in Treatment?
Ten years ago, a diagnosis of advanced pancreatic cancer meant months to live. Now, some patients are surviving years. The biggest shift? Combining treatments before surgery.
Neoadjuvant therapy - chemo before surgery - is now standard for borderline resectable tumors. The FOLFIRINOX combo (fluorouracil, leucovorin, irinotecan, oxaliplatin) shrinks tumors in over half of cases, according to the 2021 Alliance A021501 trial. That means more people become eligible for surgery, which is still the only chance at a cure.
The Whipple procedure - removing part of the pancreas, stomach, and small intestine - is no longer a last resort. At top centers, 20-25% of patients who get this surgery live five years or more. That’s better than ever. Recovery is tough, but survival is real.
For those who can’t have surgery, chemo has improved dramatically. The 2022 PRODIGE 24 trial showed that modified FOLFIRINOX nearly doubled survival compared to older drugs like gemcitabine. Median survival jumped from 20 months to over 54 months. That’s not a cure, but it’s a game-changer.
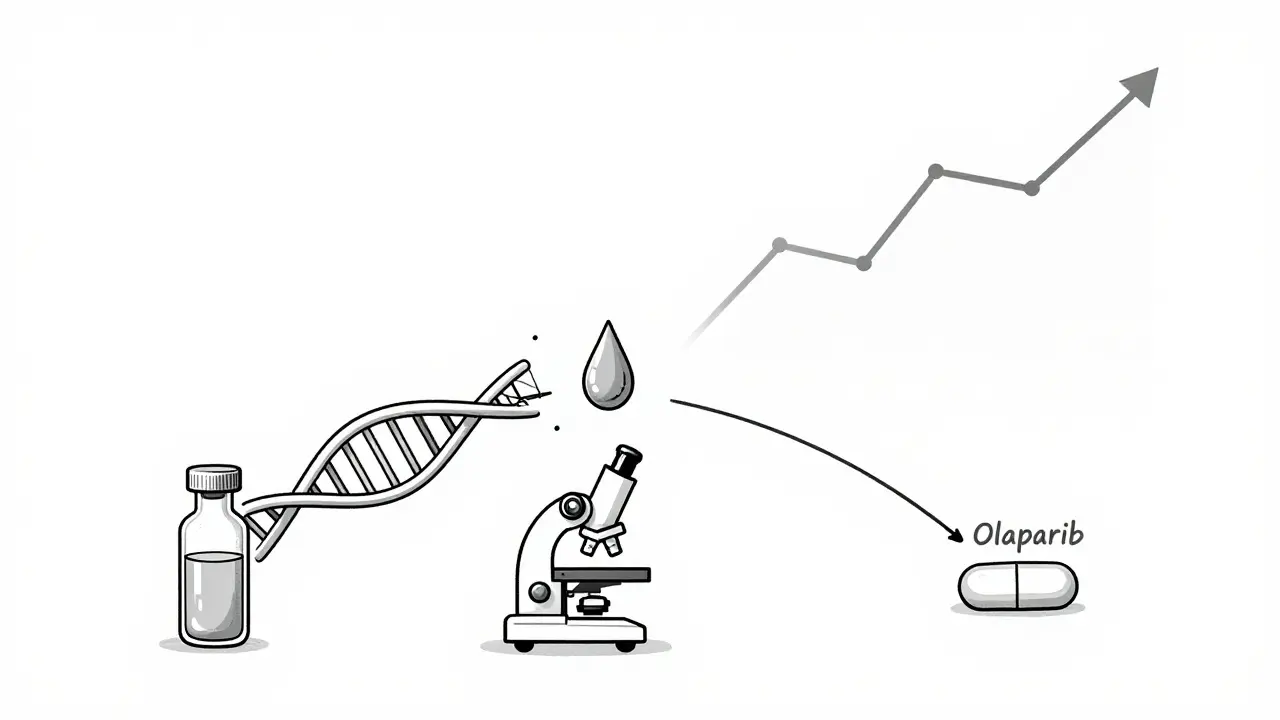
Targeted therapies are now a reality for some. If your tumor has a BRCA1 or BRCA2 mutation, the drug olaparib can slow growth for nearly eight months longer than placebo. It’s not for everyone - only about 5-7% of pancreatic cancers have these mutations - but for those who do, it’s life-changing.
Another rare group - those with MSI-H or dMMR tumors - may respond to immunotherapy like pembrolizumab. These tumors make lots of abnormal proteins that the immune system can recognize. In clinical trials, 40% of these patients saw their tumors shrink. It’s rare, but when it works, it works well.
What’s Coming Next?
The future is in catching cancer before it’s even visible on a scan. Liquid biopsies - blood tests that find tumor DNA - are getting close. Johns Hopkins developed PancreaSeq, which detected early-stage cancer with 95% accuracy in high-risk patients. The DETECTA trial is testing a blood test that looks for protein markers and tumor DNA. Early results show 85% accuracy.
AI is helping too. Google Health’s LYNA algorithm analyzed thousands of tissue slides and spotted pancreatic cancer with 99.3% accuracy. It’s not in clinics yet, but it’s a sign of where diagnostics are headed.
Even the gut microbiome is being studied. A 2023 study found that people with pancreatic cancer have different gut bacteria than healthy people. A simple stool test could one day flag risk before symptoms appear.
The National Cancer Institute aims to cut pancreatic cancer deaths by 25% by 2030. That’s ambitious. But with better detection and smarter treatments, it’s possible.
What Should You Do?
If you’re over 50 and suddenly have unexplained weight loss, new diabetes, or persistent back pain - don’t wait. Tell your doctor. Mention all your symptoms, even the ones that seem unrelated. Depression, itching, greasy stools - they all matter.
If you have a family history of pancreatic cancer or known genetic risks like BRCA mutations, ask about screening. Don’t assume it doesn’t apply to you. Early detection saves lives.
And if you’re diagnosed - don’t give up. Treatment is better than ever. Clinical trials are offering hope where there was none. Ask about genetic testing. Ask about neoadjuvant therapy. Ask about targeted drugs. You’re not just a statistic. You’re part of a growing group of people beating the odds.
Can pancreatic cancer be detected early?
Yes - but only in a small percentage of cases. Early detection is possible for people at high risk, like those with BRCA mutations or hereditary pancreatitis, through annual MRI or endoscopic ultrasound. For the general population, there’s no standard screening. However, new blood tests like PancreaSeq and the DETECTA trial show promise in catching tumors before they spread, especially in people with new-onset diabetes or unexplained weight loss.
What are the first symptoms of pancreatic cancer?
The earliest signs are often vague: unexplained weight loss, new-onset diabetes (especially after age 50), persistent upper abdominal or back pain, jaundice (yellow skin and eyes), dark urine, pale stools, loss of appetite, nausea, and severe itching. Depression or anxiety can also appear months before physical symptoms, according to research from Columbia University and the PMC study.
Is pancreatic cancer curable?
It can be - but only if caught early and the tumor hasn’t spread. Surgery, usually the Whipple procedure, is the only known cure. For patients with localized tumors who undergo surgery, 5-year survival rates are 20-25%. For those with metastatic disease, cure is rare, but treatments like modified FOLFIRINOX and targeted therapies can extend life significantly - sometimes by years.
What causes pancreatic cancer?
Most cases aren’t inherited. Smoking, obesity, chronic pancreatitis, and long-term diabetes increase risk. About 10% of cases are linked to inherited gene mutations like BRCA1, BRCA2, Lynch syndrome, or familial atypical multiple mole melanoma (FAMMM) syndrome. The exact trigger isn’t known, but mutations in the KRAS gene are found in over 90% of pancreatic tumors.
How long do people live after diagnosis?
The overall 5-year survival rate is 12%. But that number hides big differences. If the cancer is caught before it spreads, survival jumps to 44%. For those with metastatic disease, median survival is now 12-15 months with modern treatments - up from just 6 months in 2000. Some patients on advanced therapies live three to five years or longer.
Are there new treatments on the horizon?
Yes. Liquid biopsies to detect tumor DNA in blood are being tested in large trials and could soon allow screening without imaging. AI tools are improving how doctors read scans and tissue samples. New targeted drugs are in development for KRAS mutations - once considered "undruggable." Immunotherapy is expanding beyond rare MSI-H cases. The goal is to turn pancreatic cancer into a manageable chronic disease for more people.







13 Comments