Theophylline Interaction Calculator
Theophylline Clearance Calculator
Estimate how common medications affect theophylline levels and identify potential toxicity risks. Theophylline has a narrow therapeutic range (10-20 mcg/mL), and small changes in clearance can lead to serious toxicity.
Input Your Data
Most dangerous interaction. FDA reports 12.7x higher risk of serious toxicity.
Common OTC drug. Involved in nearly 29% of theophylline toxicity cases.
Lower doses (300 mg) are safer but often overlooked.
Common respiratory antibiotics. Clarithromycin is particularly risky.
Mixed evidence but significant risk in patients with heart failure.
Smoking cessation can cause levels to rise within 2 weeks.
Theophylline isn’t used as often as it once was, but when it is, getting the dose wrong can land someone in the emergency room-sometimes with fatal results. It’s a drug that’s been around since the 1920s, still prescribed for stubborn asthma and COPD cases, especially where newer inhalers aren’t available or don’t work. But here’s the catch: the difference between a safe dose and a toxic one is razor-thin. And the biggest danger isn’t the drug itself-it’s what else the patient is taking.
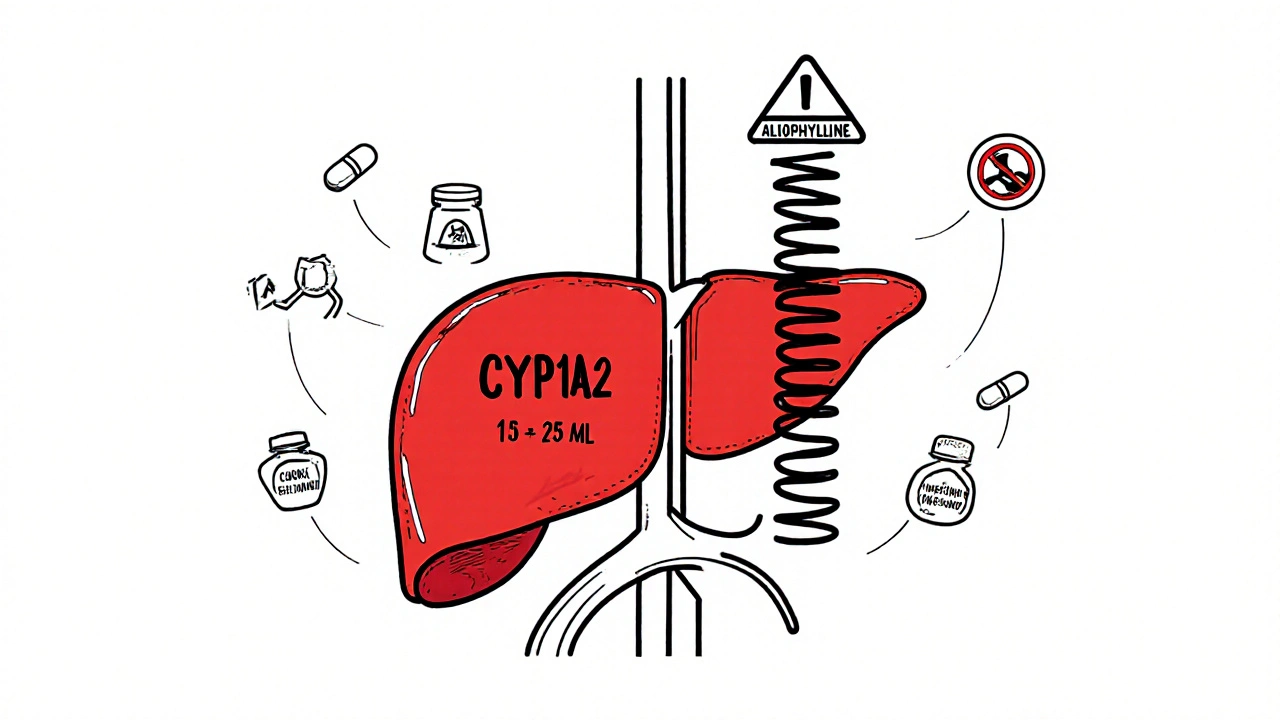
Why Theophylline Is So Fragile
Theophylline clears from the body almost entirely through the liver, using a single enzyme: CYP1A2. About 90% of it gets broken down there. That makes it incredibly sensitive to anything that slows down this enzyme. Even a small drop in clearance can send serum levels soaring. The therapeutic range? Just 10 to 20 mcg/mL. Go above 20, and you risk seizures, irregular heartbeat, or vomiting. Go above 30, and death becomes a real possibility.
What’s worse? Theophylline doesn’t follow normal dose-response rules. At therapeutic levels, its metabolism becomes saturated. That means if you increase the dose by just 10%, the blood level might jump by 30% or more. Add a drug that blocks CYP1A2, and you’re playing with fire. One patient on a stable 300 mg daily dose could start cimetidine for heartburn, and within three days, their theophylline level could spike from 15 mcg/mL to over 25 mcg/mL-straight into the danger zone.
Medications That Slow Down Theophylline Clearance
Not all drugs affect theophylline the same way. Some barely move the needle. Others are landmines. Here are the biggest offenders, based on real clinical data:
- Fluvoxamine (an SSRI antidepressant): Reduces clearance by 40-50%. This is one of the most dangerous combinations. The European Respiratory Society explicitly says to avoid it entirely. A 2021 study showed patients on both drugs had a 12.7-times higher risk of serious toxicity.
- Cimetidine (Tagamet, for heartburn): Drops clearance by 25-30%. It’s old, cheap, and still widely used. Many patients don’t even realize they’re taking it-it’s in over-the-counter stomach meds. In one 2022 hospital review, cimetidine was involved in nearly 29% of theophylline toxicity cases.
- Allopurinol (for gout): Reduces clearance by 20% at high doses (600 mg/day). Lower doses (300 mg) are safer, but many doctors don’t know that. A patient with COPD and gout might get both drugs without a single thought about interaction risk.
- Erythromycin and Clarithromycin (antibiotics): Cut clearance by 15-25%. These are common for respiratory infections. A patient with a flare-up of COPD might get azithromycin instead, which is safer-but if they get clarithromycin, the theophylline level can climb dangerously fast.
- Furosemide (Lasix, a water pill): Evidence is mixed, but some studies show a 10-15% drop in clearance. In patients with heart failure and COPD-commonly treated with both-it’s a hidden risk.
And then there are the drugs that do the opposite-speed up clearance. Phenytoin, phenobarbital, and rifampin can make theophylline useless by cutting its half-life in half. But those are easier to spot. The real danger is the quiet, everyday drugs that patients don’t think of as risky.

Real-World Consequences
In 2022, the FDA recorded over 1,800 theophylline-related adverse events in the U.S. Nearly 42% of them involved drug interactions. That’s not just numbers-it’s people. A 72-year-old man with COPD on 400 mg of theophylline daily. He starts cimetidine for acid reflux. Two days later, he’s vomiting, shaky, and his heart is racing. His serum level? 24.7 mcg/mL. He ends up in the ICU.
A 2021 study of 1,247 patients over 65 found that almost 3 out of 10 were on a medication that slowed theophylline clearance. But only 37% had their dose adjusted. Why? Because many clinicians still think, “It’s just a little bit.” But with theophylline, there’s no such thing as a little bit. A 15% drop in clearance can push someone from 18 mcg/mL to 22 mcg/mL-over the line, no warning.
Community pharmacists report the same thing. One pharmacist in Sydney shared a case where a patient came in panicked because her heart felt like it was “fluttering.” She’d started fluvoxamine for anxiety and hadn’t told her pulmonologist. Her theophylline level had jumped 60% in 10 days. She was lucky-she caught it before a seizure.
What Should You Do?
If you’re prescribing or taking theophylline, here’s what matters:
- Know the list. Memorize the big three: fluvoxamine, cimetidine, allopurinol. If a patient is on any of these, assume theophylline levels will rise.
- Check before you prescribe. Don’t just glance at the med list. Look at every new medication-OTC, supplements, antibiotics. Even herbal products like St. John’s wort can interfere.
- Test levels after changes. If you start or stop any of these drugs, check theophylline serum levels within 48 to 72 hours. Don’t wait for symptoms.
- Adjust doses early. When adding a CYP1A2 inhibitor, reduce the theophylline dose by 25-50% upfront. Don’t wait for toxicity to happen.
- Watch for smoking cessation. If a patient quits smoking, their CYP1A2 activity drops by 30-50% within weeks. That’s a hidden interaction. Many don’t realize quitting smoking can be as dangerous as adding a new drug.
The American Thoracic Society and NICE both say: avoid theophylline entirely if a patient needs long-term fluvoxamine or cimetidine. There are better, safer options now. If you’re stuck with theophylline because of cost or access, treat it like insulin-tiny changes matter.

Why This Still Matters in 2025
Theophylline use has dropped by over 60% in the U.S. since 2000. But that doesn’t mean the risk is gone. It’s actually growing. The remaining patients are older, sicker, on more medications. They’re the ones with heart failure, gout, depression, and chronic infections-all conditions that bring in the drugs that mess with theophylline.
And here’s the kicker: electronic health records rarely flag these interactions well. A 2023 survey of 412 pulmonologists found that 62% said their EHR didn’t give them a strong enough warning when theophylline was paired with cimetidine or fluvoxamine. That means the burden falls on the clinician-and often, it’s missed.
Global use is still around 3% of COPD maintenance therapy, but it’s 12% in parts of Africa and 8% in Asia. In low-resource settings, theophylline is often the only affordable option. That makes understanding these interactions not just important-it’s life-or-death.
There’s new research into low-dose theophylline for anti-inflammatory effects in COPD. But those trials exclude anyone on CYP1A2 inhibitors. Why? Because the risk isn’t worth it. And if the researchers know it, so should you.
Bottom Line
Theophylline isn’t a drug you use lightly. It’s not a first-line choice anymore. But when it’s needed, it can save lives-if you manage it right. The biggest threat isn’t the disease. It’s the pills patients take for other things. Cimetidine. Fluvoxamine. Allopurinol. These aren’t rare drugs. They’re common. And together with theophylline, they’re a quiet recipe for disaster.
If you’re on theophylline, ask your doctor: “Could anything I’m taking be making this more dangerous?” If you’re prescribing it, don’t assume the patient knows. Don’t assume the system will warn you. Check the list. Check the levels. Adjust early. Because with theophylline, there’s no second chance.
Can I take ibuprofen with theophylline?
Yes, ibuprofen does not significantly affect theophylline clearance. It doesn’t inhibit CYP1A2 or CYP3A4 in a way that changes theophylline levels. Most NSAIDs like ibuprofen, naproxen, or celecoxib are considered safe to use with theophylline. However, always monitor for side effects like nausea or jitteriness, as both drugs can irritate the stomach.
What happens if I stop smoking while on theophylline?
Stopping smoking can cause theophylline levels to rise by 30-50% within two weeks. Smoking induces CYP1A2, so when you quit, the enzyme activity drops. If your dose was set while you were smoking, you may suddenly have toxic levels. Always tell your doctor if you quit smoking-they’ll likely need to lower your theophylline dose and recheck your blood level within 5-7 days.
Is theophylline still used today?
Yes, but only in specific cases. It’s mostly used for severe asthma or COPD that doesn’t respond to inhalers, especially in places where newer drugs are too expensive. In the U.S., it’s prescribed in less than 2% of COPD cases. But in parts of Asia and Africa, it’s still used in over 10% of patients because it’s cheap and effective when other options aren’t available.
How often should theophylline levels be checked?
Check levels when starting the drug, after any dose change, and within 48-72 hours after starting or stopping any new medication-especially antibiotics, antidepressants, or heartburn drugs. Also check after quitting smoking or if you develop symptoms like nausea, palpitations, or tremors. Routine checks every 3-6 months are recommended for stable patients, but only if no new drugs are added.
Are there safer alternatives to theophylline?
Yes. For asthma and COPD, inhaled bronchodilators like salmeterol, formoterol, or tiotropium are safer, more effective, and have far fewer interactions. Inhaled corticosteroids combined with long-acting bronchodilators are now first-line. Theophylline is reserved for cases where these don’t work or aren’t accessible. If you’re on theophylline, ask if switching to an inhaler is an option.







12 Comments