Pregnancy Medication Safety Checker
Check Your Medication Safety
See if your medication has pregnancy registry data and learn about its safety profile
Pregnancy Registry Status:
Key Findings:
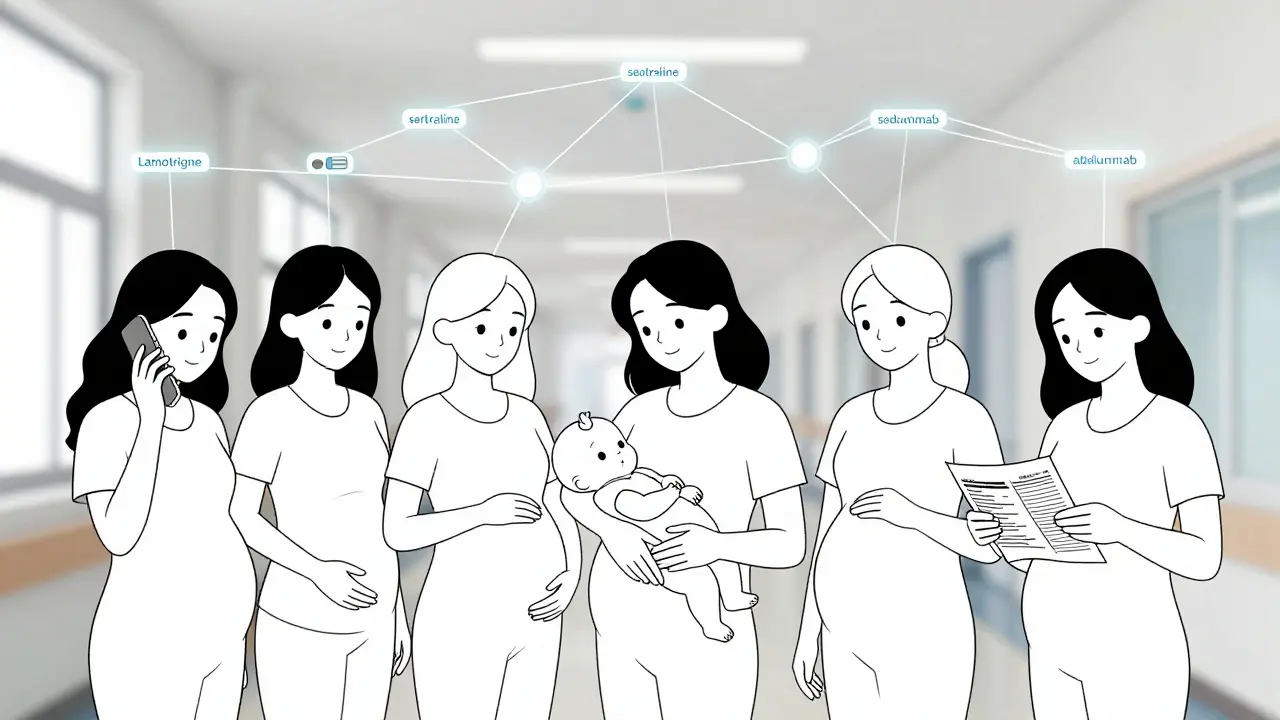
When you’re pregnant and need to take a medication - whether it’s for depression, epilepsy, asthma, or an autoimmune condition - the question isn’t just "Will this help me?" It’s "Will this hurt my baby?" For decades, doctors had no solid answers. Clinical trials rarely included pregnant women, leaving a dangerous gap in knowledge. That’s where pregnancy registries come in. These aren’t just databases. They’re lifelines built by real women who volunteer to share their stories so future moms can make safer choices.
Why Pregnancy Registries Exist
After the thalidomide disaster in the 1960s, when thousands of babies were born with severe limb defects linked to a morning sickness drug, the medical world realized it couldn’t wait until harm was done to act. Since then, regulators like the FDA and EMA have required drug makers to set up pregnancy registries for medications likely to be used by women of childbearing age. These registries track what happens when a pregnant woman takes a specific drug - not just the immediate outcome, but long-term effects on the child.Here’s the reality: about 80% of pregnant women in the U.S. take at least one medication during pregnancy. Some are essential. Others are taken out of caution. Without registries, we’d be flying blind. Pre-approval trials don’t include pregnant people for ethical reasons. So the only way to know if a drug causes birth defects is to watch what happens after it hits the market - and that’s exactly what these registries do.
How Pregnancy Registries Work
These aren’t passive systems. They’re active, structured studies. When a woman finds out she’s pregnant and is taking a medication covered by a registry, she can enroll. Registry staff - often nurses or researchers - contact her soon after. They ask detailed questions: What drug? What dose? When did you start taking it? Are you taking anything else? Do you smoke? Have you had previous pregnancies?Then they follow her through the entire pregnancy. They record whether the baby was born prematurely, if there was a miscarriage, what the birth weight was, and whether any major physical abnormalities were detected. Some registries go further - tracking developmental milestones at 6 months, 12 months, even 2 years after birth. The National Pregnancy Registry for Psychiatric Medications, for example, follows children up to age one to check for delays in motor skills or speech.
Unlike emergency reports or insurance claims, registries collect data before outcomes are known. That’s key. It cuts down on memory errors. A woman doesn’t have to guess what she took six months ago - she’s asked right away. This makes the data far more reliable than retrospective studies.
What We’ve Learned So Far
Registries have given us real, usable answers - not just guesses.Take lamotrigine, a common anti-seizure drug. Early fears suggested it might cause cleft lip or palate. But data from multiple registries showed no increased risk. Today, it’s considered one of the safer options for pregnant women with epilepsy.
For antidepressants like sertraline, registries helped calm fears. While early studies hinted at possible heart defects, larger registry data showed the risk, if any, was extremely low - lower than the baseline risk in the general population. That’s huge. It means doctors can now tell women with severe depression: "Your mental health matters too. This medication is likely safe."
On the flip side, registries confirmed risks we suspected. For example, isotretinoin (Accutane) for acne was already known to be dangerous, but registries documented exactly how common severe birth defects were - and helped push stronger warnings and mandatory pregnancy testing before prescribing.
Biologics - newer, complex drugs used for conditions like rheumatoid arthritis or Crohn’s - are another big area. Before registries, we had almost no data. Now we know that drugs like adalimumab (Humira) and certolizumab (Cimzia) don’t appear to increase major birth defect rates. That’s changed how doctors manage autoimmune diseases in pregnancy.
The Limits of Registries
Don’t mistake registries for perfect science. They have serious constraints.First, they’re small. Most registries enroll fewer than 500 women. To detect a rare defect that affects 1 in 100 babies, you’d need over 1,200 exposed pregnancies to be statistically sure. Most registries never hit that number. That means they’re great at spotting big risks - like a drug causing a pattern of severe defects - but terrible at catching small increases in risk, like a 20% higher chance of a mild heart issue.
Second, enrollment is voluntary. Only about 15-20% of eligible women sign up. Those who do are often more anxious, more informed, or more motivated to help. That can skew results. If only highly worried women enroll, the data might look worse than it is.
Third, they can’t prove safety - only absence of harm. A registry might show no birth defects in 300 women who took Drug X. That doesn’t mean Drug X is 100% safe. It just means, based on the data so far, it doesn’t cause major defects at a rate higher than expected. The message is: "We haven’t seen a red flag yet."
Who Runs These Registries?
Most are run by hospitals or research centers, often in partnership with drug companies. The FDA doesn’t run them directly, but it requires them as part of drug approval. The EMA does the same in Europe.Examples include:
- National Pregnancy Registry for Psychiatric Medications - run by Massachusetts General Hospital, tracks over 45 drugs including SSRIs, SNRIs, and antipsychotics.
- MotherToBaby - operates multiple registries across the U.S., funded by pharmaceutical sponsors but staffed by trained specialists who provide free counseling to participants.
- Antiepileptic Drug Pregnancy Registry - focused on seizure medications, one of the longest-running and most influential registries.
These organizations don’t just collect data. They give back. Women who enroll get personalized updates, safety summaries, and direct access to experts. Many say that’s the biggest reason they participate - not to help science, but to get answers for themselves.
The Emotional Side of Participation
It’s easy to talk about data. But behind every number is a woman who’s scared.Women taking psychiatric medications often describe feeling trapped. "If I stop my antidepressant, I might spiral. If I keep taking it, I might hurt my baby." Registry staff hear this daily. One woman told a researcher: "I didn’t enroll because I thought it would help science. I enrolled because I needed to know I wasn’t the only one feeling this way."
Registration doesn’t give instant reassurance. It takes months - sometimes years - to see results. That’s frustrating. Some women drop out because they’re anxious and don’t get immediate answers. Registry teams now train staff to manage expectations: "We’re not here to say if it’s safe. We’re here to find out."
Despite that, 78% of women who complete participation say they’re glad they joined. They feel empowered. They feel heard. And they feel like they’ve helped other mothers.
What’s Next for Pregnancy Registries?
The field is evolving. The FDA launched the Pregnancy Safety Research Network in 2022 to link registries together. That means data from 10 different registries on antidepressants can now be pooled - increasing sample size and power.There’s also a push to integrate registry data with electronic health records. Instead of relying on phone calls and paper forms, future registries might pull data directly from doctor’s notes, pharmacy fills, and lab results - making it faster, more accurate, and less burdensome for participants.
Experts now agree: registries alone aren’t enough. The future is hybrid. Combine small, detailed registries with big, real-world data from insurance claims or hospital records. Use registries to spot signals, then use large databases to measure the actual risk.
For now, though, they’re still the best tool we have. Especially for rare diseases, new biologics, or drugs used by only a few thousand women each year. Without registries, we’d have no data at all.
What You Should Do If You’re Pregnant and Taking Medication
If you’re pregnant and on a medication - even one you’ve taken for years - here’s what to do:- Don’t stop cold. Stopping suddenly can be riskier than continuing. Talk to your doctor.
- Ask if there’s a pregnancy registry for your medication. Your OB, pharmacist, or even the drug manufacturer’s website might have info.
- Consider enrolling. It’s free. It’s voluntary. You’ll get personalized updates. And you’ll help others.
- Use MotherToBaby. They offer free, confidential counseling at 1-866-626-6847 or through their website. They run several registries and can help you decide if you qualify.
There’s no perfect answer when it comes to medication in pregnancy. But we’re learning faster than ever - thanks to the courage of women who step forward to share their stories.
Are pregnancy registries safe to join?
Yes. Participation is completely voluntary and confidential. Registries follow strict privacy rules, and your personal health information is never shared with drug companies or insurers. Only de-identified data is used for research. You can withdraw at any time.
Can a registry tell me if my medication is safe right now?
No. Registries collect data over time and analyze it later. They can’t give you instant answers. If you need immediate advice, talk to your doctor or call MotherToBaby. Registries are for building long-term evidence, not emergency counseling.
Do I need to be in a clinical trial to join a registry?
No. Registries are for women who are taking a medication as prescribed - not part of a research study. You don’t need to be enrolled in a trial. If your drug is covered by a registry and you’re pregnant, you can sign up just by contacting the registry directly.
How long does it take to get results from a registry?
It can take several years. Registries need enough participants and enough time for babies to be born and followed up. Most findings are published after 3-5 years of data collection. Some studies take longer if the drug is rarely used or if long-term child development is being tracked.
Are pregnancy registries only in the U.S.?
No. Similar registries exist in Europe, Canada, Australia, and other countries. The European Medicines Agency requires them for many new drugs. Global collaboration is growing, and data is often shared between countries to improve accuracy.








14 Comments