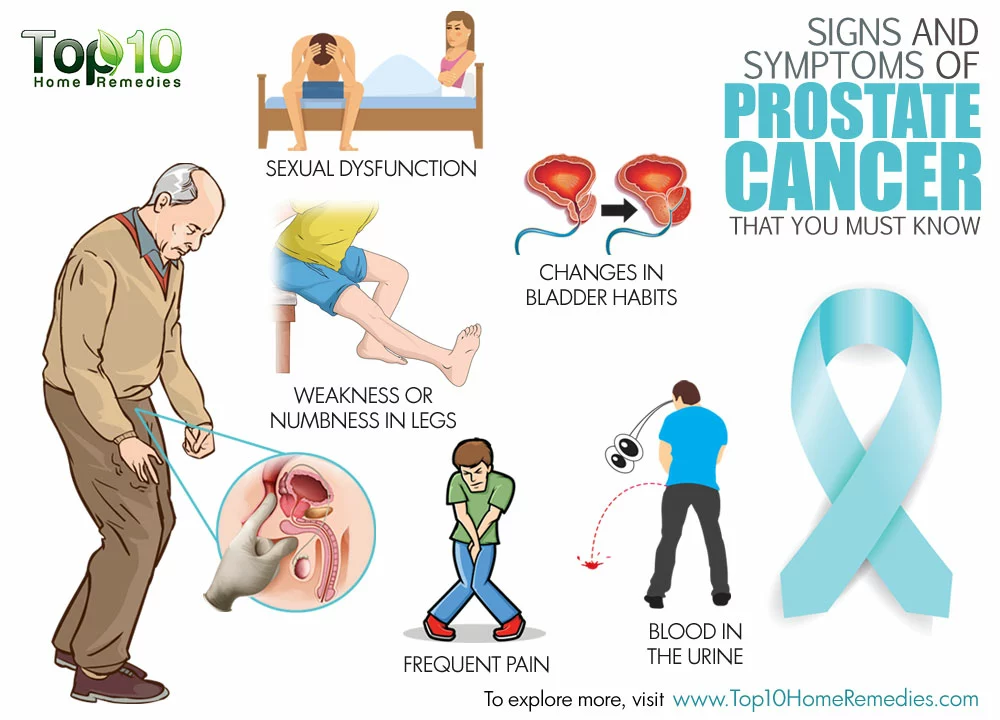
When you’re on diabetes medication, what you eat doesn’t just affect your energy-it can make your pills work better or worse. A sugary snack might seem harmless, but if you’re taking metformin, sulfonylureas, or insulin, that bite could send your blood sugar soaring-or crash it too low. The truth is, sugar intake isn’t just about weight or cravings. It’s a direct player in how well your medication controls your blood sugar.
Why Sugar Changes How Medications Work
Diabetes medications don’t work in a vacuum. They’re designed to balance your body’s glucose levels, but they can’t fight off a sugar overload. Metformin, the most common first-line drug for Type 2 diabetes, works by reducing liver glucose production and helping muscles absorb sugar better. But if you’re eating 100 grams of added sugar a day-about eight teaspoons of sugar in soda, yogurt, and snacks-your body is flooded with glucose faster than metformin can manage. A 2022 GoodRx analysis found patients on high-sugar diets needed 28% more metformin just to reach the same blood sugar levels as those limiting sugar to under 25 grams daily.Medications That Are Especially Sensitive to Sugar
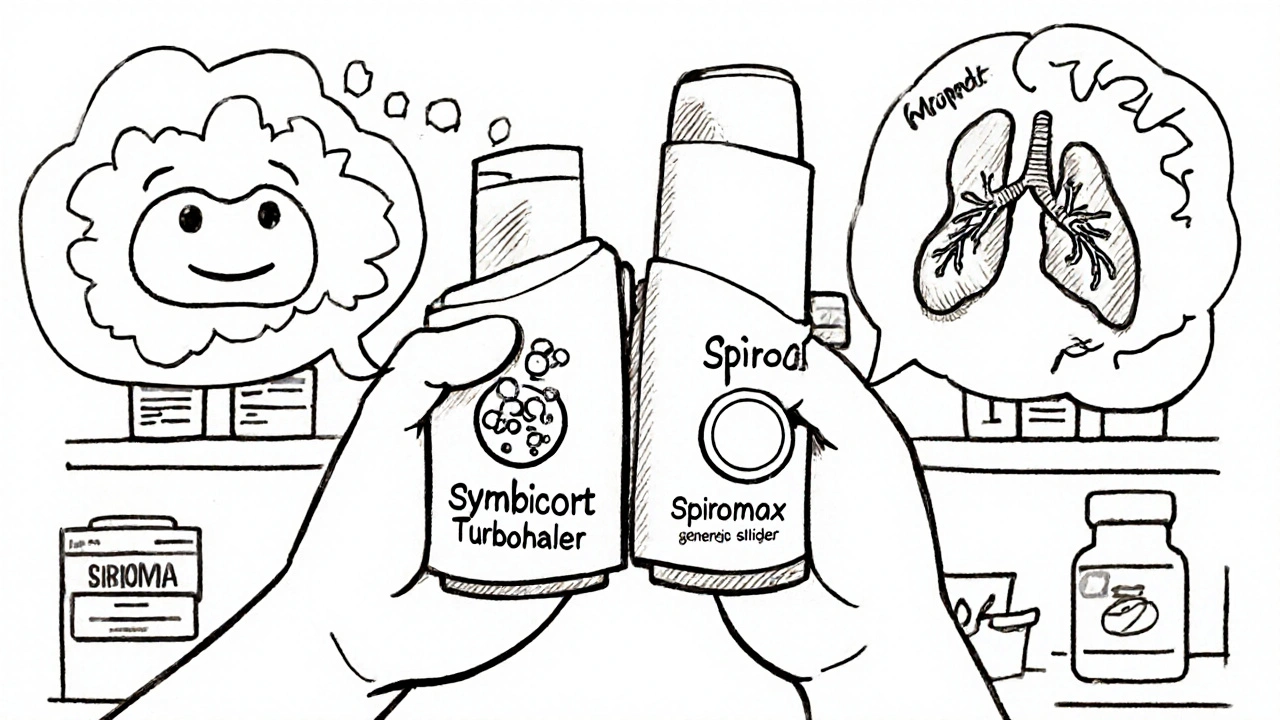
Not all diabetes drugs react the same way to sugar. Some are more forgiving. Others? They’re like a tightrope walker with no safety net.- Sulfonylureas (like glipizide and glyburide) and meglitinides (like repaglinide) force your pancreas to pump out insulin. If you skip a meal or eat too little sugar, you risk low blood sugar. But if you eat a huge sugary meal? Your body gets hit with too much insulin all at once, and then crashes hours later. The Cleveland Clinic reports 68% of patients on glyburide had dangerous hypoglycemia after one high-sugar meal.
- Insulin requires precise carb counting. Even with smart pumps, inconsistent sugar intake leads to wild swings. Data from the T1D Exchange shows patients who logged every carb had HbA1c levels 0.8% lower than those who didn’t.
- Metformin doesn’t cause low blood sugar on its own, but high sugar and high fat meals slow how fast it’s absorbed. One study showed peak levels dropped by up to 30% after a sugary, fatty meal.
- SGLT2 inhibitors (like dapagliflozin) and GLP-1 agonists (like semaglutide) are more forgiving. They work by flushing sugar out through urine or slowing digestion. But even they lose 15-20% of their power if you regularly eat over 100g of added sugar daily.
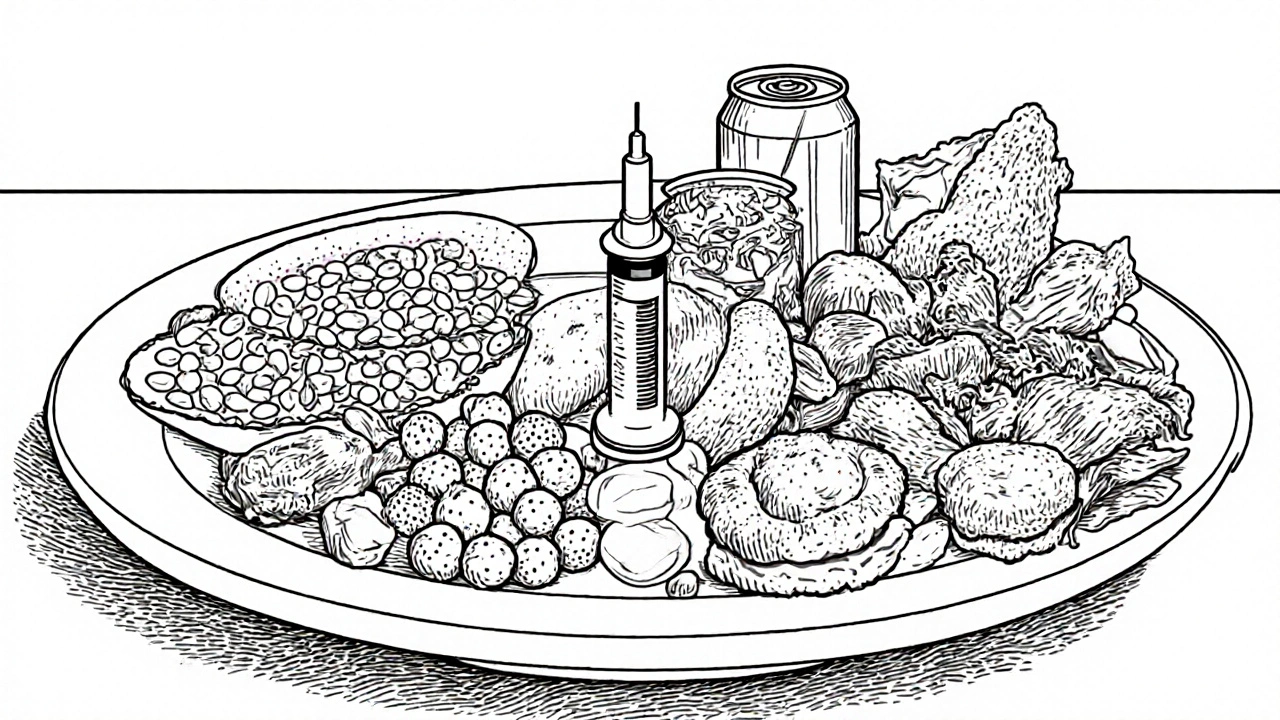
What Foods to Avoid With Diabetes Medications
It’s not just about sugar. It’s about how sugar is delivered-and what else comes with it.The GoodRx 2023 clinical review flagged seven food categories that interfere with diabetes meds:
- Sugary drinks-soda, sweetened tea, fruit juice with more than 20g sugar per serving. These spike blood sugar faster than solid food. The NHS says you need to check your glucose every 2 hours for 6 hours after drinking one.
- High-sugar fruits-mangoes, grapes, cherries. They’re natural, but a cup of grapes has 23g of sugar. Eat them with protein or fat to slow absorption.
- Processed foods-granola bars, flavored yogurts, sauces. Check labels. If it has more than 15g added sugar per serving, it’s a red flag.
- High-fat meals-fried chicken, creamy pasta, butter-heavy dishes. Fat delays stomach emptying, which messes with how fast metformin and other drugs get absorbed.
- Alcohol-especially sweet cocktails. A margarita can pack 30g of sugar and lower blood sugar hours later, especially if you’re on insulin or sulfonylureas.
- Refined carbs-white bread, pastries, crackers. They break down into glucose fast. A single slice of white bread can have 15g of carbs with no fiber to slow the spike.
What You Should Eat Instead
You don’t need to eliminate sugar. You need to manage it.The 2025 International Journal of Molecular Sciences review found that low-glycemic-index (GI) foods-those with a GI under 55-boost insulin sensitivity by 25-40%. That means your body uses insulin better, and your meds work more efficiently.
Choose:
- Whole grains: oats, quinoa, barley
- Legumes: lentils, chickpeas, black beans
- Non-starchy vegetables: broccoli, spinach, peppers
- Low-sugar fruits: berries, apples, pears
- Healthy fats: avocado, nuts, olive oil
Pair carbs with protein or fat. Eat an apple with peanut butter. Have oatmeal with chia seeds and almonds. These combos slow digestion, flatten glucose spikes, and make your medication’s job easier.
How Much Sugar Is Too Much?
The American Diabetes Association recommends limiting added sugar to less than 10% of your daily calories. For a 2,000-calorie diet, that’s about 50 grams of added sugar-roughly 12 teaspoons.But here’s the catch: most people don’t realize how fast that adds up.
- One 12-oz soda = 39g sugar
- One flavored yogurt = 18g sugar
- One granola bar = 15g sugar
- One tablespoon of ketchup = 4g sugar
That’s already 76g before lunch. No wonder blood sugar stays high-even with meds.

What About Other Medications?
Diabetes meds don’t live alone. Many people take other drugs that can make sugar control harder.- Prednisolone (a steroid) can raise blood sugar by 50-100 mg/dL within a day.
- Furosemide (a water pill) may need metformin dose adjustments in over a third of users.
- Hormonal birth control changes how the body handles glucose in nearly 3 out of 10 women.
If you’re on any of these, talk to your doctor. Your sugar targets and medication doses might need tweaking.
The Real Game-Changer: Nutrition Counseling
You wouldn’t expect a car to run well without tuning. Yet, many people start diabetes meds without any dietary guidance.A 2024 analysis from the American Association of Clinical Endocrinologists found that patients who got nutrition counseling alongside their meds reached their HbA1c target in 6.2 months-almost five months faster than those who didn’t. The Cleveland Clinic’s data shows patients who completed their 12-week nutrition program had 63% fewer emergency visits and needed 2.5 fewer medication changes in their first year.
And yet, only 39% of primary care doctors refer new patients to dietitians. The ADA says everyone starting diabetes meds should see a registered dietitian within 30 days. But only 42% of healthcare systems actually do it.
It’s Not About Perfection-It’s About Consistency
You don’t need to be a nutrition expert. You don’t need to cut out sugar forever. But you do need to be consistent.Try this:
- Track your sugar for one week using a free app like MyFitnessPal.
- Look for patterns. Do your highs happen after lunch? After coffee with syrup?
- Swap one sugary item per day for a low-GI alternative.
- Always eat carbs with protein or fat.
- Check your blood sugar 2 hours after meals for a week. See how your body reacts.
Continuous glucose monitors (CGMs) show that people on metformin who eat high-sugar meals spend 47% more time in high blood sugar than those who don’t. That’s not just inconvenient-it’s damaging your kidneys, nerves, and eyes over time.
Medications are powerful. But they’re not magic. Sugar intake is the silent variable that can make or break your treatment. The science is clear: manage your sugar, and your meds will work better. Skip it, and you’re fighting an uphill battle-every single day.
Can I still eat fruit if I have diabetes and take medication?
Yes, but choose wisely. Berries, apples, pears, and citrus fruits have lower sugar and more fiber than mangoes, grapes, or watermelon. Eat them with a source of protein or fat-like a handful of almonds or a spoon of Greek yogurt-to slow sugar absorption. A half-cup of blueberries (15g carbs) is a safe portion. Avoid fruit juice entirely-it’s sugar without fiber and spikes blood sugar fast.
Does metformin stop me from gaining weight?
Metformin can help with modest weight loss or prevent weight gain, but only if you’re not overloading on sugar and refined carbs. If you eat a lot of high-sugar foods, metformin can’t compensate. Studies show patients who pair metformin with low-sugar, low-refined-carb diets lose 3-5% of their body weight in 6 months. Without dietary changes, weight gain is still likely.
Why does my blood sugar spike even when I take my meds?
Your meds might be working, but your sugar intake is overwhelming them. High-sugar meals-especially from drinks, snacks, or processed foods-cause rapid glucose spikes that even the best medications can’t fully control. A 2023 study showed patients on metformin who ate over 100g of added sugar daily had 2.3 times more high-blood-sugar episodes than those under 50g. Check your portions, track your sugar, and look for hidden sources.
Can I drink alcohol with my diabetes medication?
Moderate alcohol is okay for some, but it’s risky. Sweet cocktails, wine coolers, and beer can have 20-40g of sugar. Alcohol also blocks the liver from releasing glucose, which can cause delayed low blood sugar-especially if you’re on insulin or sulfonylureas. If you drink, choose dry wine, light beer, or spirits with soda water. Never drink on an empty stomach, and check your blood sugar before bed.
Do I need to see a dietitian if I’m on diabetes meds?
Yes. The American Diabetes Association recommends medical nutrition therapy within 30 days of starting diabetes meds. Dietitians help you personalize your plan based on your meds, lifestyle, and preferences. Patients who see a dietitian reach their HbA1c goals nearly 50% faster and have far fewer emergencies. If your doctor didn’t refer you, ask for one. It’s a covered benefit under most insurance plans.
Are newer diabetes drugs better for sugar control?
SGLT2 inhibitors and GLP-1 agonists are more consistent across different sugar intakes because they don’t rely on insulin. SGLT2 drugs flush sugar out through urine, and GLP-1 drugs slow digestion and reduce appetite. But even they lose effectiveness if you regularly eat over 100g of added sugar daily. No medication replaces smart eating. The newest drugs still work best with a low-sugar diet.






10 Comments