Age-Related Dosing: How Medication Needs Change as You Get Older
When you’re younger, a standard dose of a medication often works fine. But as you age, your body changes—your kidneys don’t filter as well, your liver processes drugs slower, and your muscle mass decreases while fat increases. This means age-related dosing, the practice of adjusting medication amounts based on age, kidney function, and metabolism. Also known as geriatric dosing, it’s not just a suggestion—it’s often a safety requirement. Many seniors take five or more prescriptions daily, and without proper dose adjustments, they’re at higher risk for side effects like dizziness, confusion, falls, and even hospitalization.
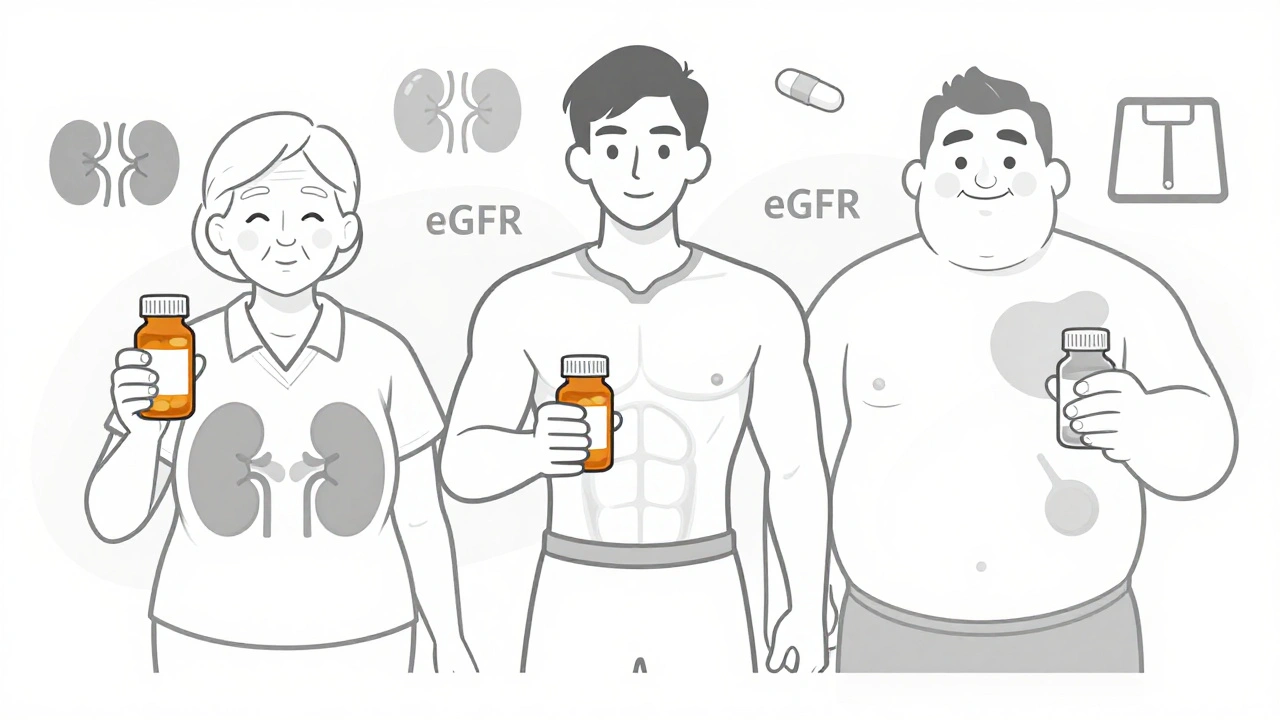
Renal dosing, how kidney function determines how much of a drug stays in your system. Also known as kidney-based dosing, it’s one of the most critical factors in age-related dosing. As we get older, eGFR (estimated glomerular filtration rate) drops naturally—even if you don’t have kidney disease. Drugs like lisinopril, metformin, and many antibiotics rely on kidney clearance. If your doctor doesn’t check your eGFR, you might be taking too much. The same goes for drug interactions, when two or more medications affect each other’s behavior in the body. Also known as medication conflicts, they become more dangerous with age because seniors are more likely to be on multiple drugs. Think of anticholinergics like Benadryl or oxybutynin—they can cause memory fog and increase dementia risk, yet they’re still prescribed to older adults for bladder issues. Or theophylline, which can turn toxic if taken with common antibiotics. These aren’t edge cases—they’re routine risks.
Elderly pharmacology, the study of how drugs behave in older bodies and how to use them safely. Also known as geriatric pharmacology, it’s the science behind why a 30-year-old can take a full dose of a painkiller while a 75-year-old might need half—or none. It’s not about being frail. It’s about biology. Your body isn’t broken—it’s just different. That’s why senior patient education matters. You need to know what your meds do, why the dose changed, and when to speak up about side effects. Many older adults don’t realize that dizziness on blood pressure meds or dry mouth from anticholinergics aren’t normal aging—they’re red flags.
What you’ll find below isn’t just a list of articles. It’s a practical toolkit. You’ll learn how to spot dangerous interactions in your medicine cabinet, understand why your doctor might lower your dose, and find out which common drugs are riskiest for seniors. From how to read supplement labels to why kidney disease changes everything, these posts cut through the noise and give you real, actionable info. No fluff. Just what you need to stay safe, sharp, and in control of your health as you age.