Getting the right dose of medication isn’t just about following the label. For many people, the standard dose on the bottle could be too much-or too little-depending on their age, weight, or how well their kidneys are working. A 70-year-old with kidney disease and a 25-year-old athlete might both be prescribed the same drug, but their bodies handle it completely differently. This isn’t guesswork. It’s science. And getting it wrong can mean the difference between healing and hospitalization.
Why One Size Doesn’t Fit All
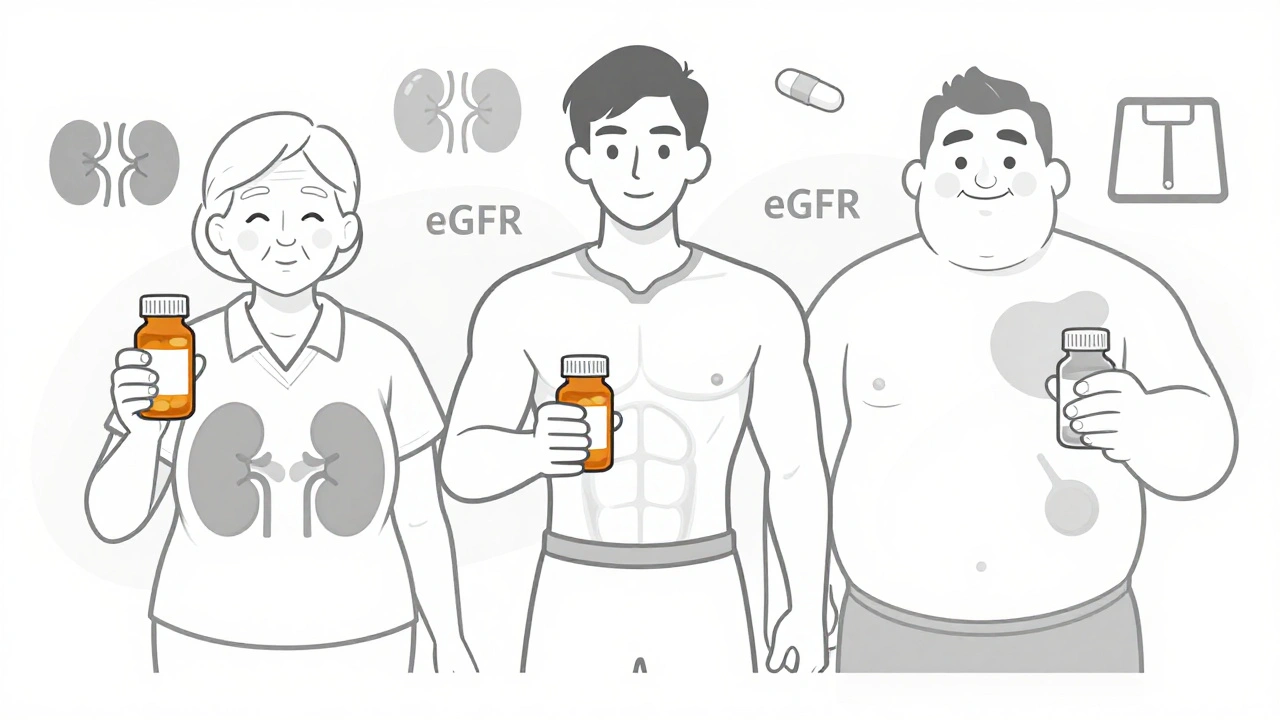
Most drug labels list a standard dose based on a healthy adult weighing around 70 kg with normal kidney function. But that’s not most people. About 37 million American adults have chronic kidney disease (CKD). One in four people over 65 has reduced kidney function. And nearly one-third of U.S. adults are obese. If you fall into any of those groups, your body processes drugs differently. Too much drug builds up and causes side effects-dizziness, confusion, kidney damage, even seizures. Too little, and the drug doesn’t work. That’s why dosing adjustments aren’t optional. They’re essential for safety.How Kidney Function Changes Everything
Your kidneys filter about 120-150 quarts of blood every day. That’s how they remove drugs and waste. When kidney function drops, those drugs stick around longer. Some medications, like antibiotics, painkillers, and diabetes drugs, are cleared mostly by the kidneys. If your kidneys aren’t working well, even a normal dose can become toxic. Doctors don’t just look at your serum creatinine level. They calculate your estimated glomerular filtration rate (eGFR) using the CKD-EPI equation. This gives a clearer picture of how well your kidneys are filtering. Here’s how it breaks down:- eGFR ≥90: Normal kidney function
- eGFR 60-89: Mild reduction
- eGFR 45-59: Mild to moderate reduction
- eGFR 30-44: Moderate to severe reduction
- eGFR 15-29: Severe reduction
- eGFR <15: Kidney failure
Weight Matters-More Than You Think
Weight affects how drugs spread through your body. If you’re underweight, a standard dose might flood your system. If you’re obese, the drug might not reach enough tissue to work. But you don’t just use your actual weight. For people with a BMI over 30, doctors use adjusted body weight. Here’s how it works:- Calculate ideal body weight (IBW):
- Men: 50 kg + 2.3 kg for each inch over 5 feet
- Women: 45.5 kg + 2.3 kg for each inch over 5 feet
- Adjusted weight = IBW + 0.4 × (actual weight − IBW)
Age Isn’t Just a Number
As you get older, your kidneys naturally lose function-even if you’re healthy. Muscle mass declines, which lowers creatinine production. That can make your serum creatinine look normal when your kidneys are actually slowing down. The CKD-EPI equation accounts for this by factoring in age and sex. But many older adults still get standard doses because providers assume their labs are “normal.” Studies show that 30% of adverse drug events in older adults are tied to kidney-related dosing errors. Drugs like metformin, digoxin, and certain antibiotics are especially risky. For example, metformin is often stopped if eGFR drops below 30, but many patients stay on it at higher levels without proper monitoring. That’s why guidelines now recommend reducing metformin to 500 mg daily if eGFR is between 30-45.Real-World Mistakes and How to Avoid Them
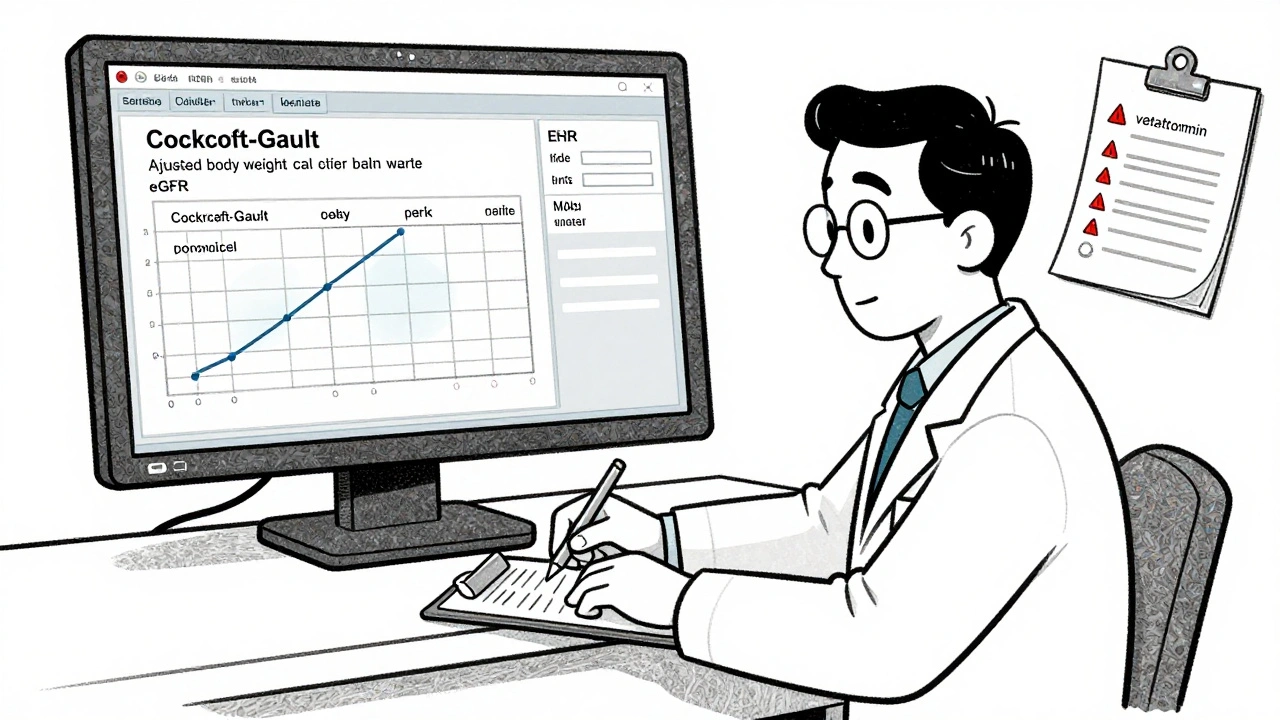
A pharmacist in Ohio caught a patient on 1000 mg of metformin twice daily with an eGFR of 28. That’s three times the safe dose. Another patient got a full dose of vancomycin despite having Stage 3B CKD-and ended up with hearing loss because the drug built up. These aren’t rare. A 2022 survey found that 68% of pharmacists see incorrect renal dosing at least once a week. The biggest problem? Inconsistent guidelines. One hospital says to reduce cefazolin by 50% at eGFR 20-29. Another says 75%. One reference says to use CrCl. Another says to use eGFR. That confusion leads to errors. Here’s how to cut down on mistakes:- Always calculate CrCl using Cockcroft-Gault for dosing decisions, not just rely on eGFR.
- Use adjusted body weight for patients with BMI >30.
- Check the drug’s label or a trusted source like Lexicomp or Micromedex for specific renal dosing rules.
- When in doubt, reduce the dose or extend the dosing interval-better safe than sorry.
- Ask for a pharmacist consult. They’re trained to spot these issues.
Technology Is Helping-But Not Everywhere
Hospitals with electronic health records (EHRs) that automatically calculate CrCl and flag risky doses have seen 47-53% fewer medication errors. Epic and Cerner now include built-in renal dosing tools. But not every clinic has them. Primary care doctors, emergency rooms, and nursing homes still rely on paper charts and memory. A 2023 study found that 38% of antibiotic dosing guidelines contradict each other across different sources. That’s why you need to know which reference you’re using-and why you should always double-check.What You Can Do
If you’re on any regular medication and you’re over 65, overweight, or have diabetes or high blood pressure, ask your doctor or pharmacist:- “Is my kidney function being checked?”
- “Does my dose need to change based on my weight or age?”
- “Can you show me the specific guideline you’re using for this drug?”
The Bottom Line
Medication dosing isn’t one-size-fits-all. Age, weight, and kidney function aren’t just background details-they’re core parts of your treatment plan. Ignoring them isn’t negligence. It’s dangerous. The tools to get it right exist. The knowledge is available. What’s missing is consistent use. The goal isn’t just to avoid side effects. It’s to make sure your medication actually works. That means the right dose, for your body, at the right time. And that’s something no label can tell you alone.How do I know if my medication dose needs to be adjusted for kidney function?
Your doctor should check your kidney function with a blood test for creatinine and calculate your eGFR or CrCl. If your eGFR is below 60 mL/min/1.73m² or your CrCl is below 50 mL/min, most medications that are cleared by the kidneys need adjustment. Check your drug’s label or ask your pharmacist for specific guidelines. Never assume your dose is safe just because it’s the standard.
Should I use my actual weight or ideal weight for dosing calculations?
If your BMI is over 30, use your adjusted body weight-not your actual weight. For people with low body weight (BMI under 18.5), actual weight is usually used because ideal weight formulas can overestimate kidney function. For most people with normal weight, actual weight is correct. Always confirm which weight your provider is using for calculations.
Why do some sources say to use eGFR and others say CrCl?
eGFR is better for diagnosing and staging chronic kidney disease. CrCl is better for drug dosing because most drug studies and FDA guidelines were developed using CrCl. Many hospitals now use both: eGFR for diagnosis and CrCl for dosing. Always follow the drug-specific recommendation-if it says to use CrCl, use CrCl. Don’t substitute eGFR unless instructed.
What are the most common drugs that need kidney adjustments?
Common drugs requiring renal adjustments include metformin, vancomycin, cefazolin, digoxin, lisinopril, furosemide, gabapentin, and many antibiotics and painkillers. Diabetes medications, heart failure drugs, and seizure medications are also high-risk. Always check the prescribing information for your specific drug-about 40-60% of commonly used medications need some form of adjustment in kidney disease.
Can I just reduce my dose by half if I have kidney disease?
No. That’s a common mistake. Some drugs need a 50% reduction at eGFR 30-59, others need a 75% reduction. Some need longer intervals instead of lower doses. Some shouldn’t be used at all. Reducing by half without knowing the drug’s properties can lead to underdosing or toxicity. Always follow the specific recommendation for your drug, not a general rule.






10 Comments