If you have irritable bowel syndrome, especially the constipation-predominant type (IBS-C), you’ve probably heard of bisacodyl. It’s not a cure, but for many people, it’s one of the few things that actually helps get things moving when nothing else does. Unlike fiber supplements or probiotics that take weeks to show results, bisacodyl works fast-often within 6 to 12 hours. But that speed comes with trade-offs. Understanding how bisacodyl fits into IBS management isn’t just about knowing when to take it. It’s about knowing when not to.
What Bisacodyl Actually Does in Your Gut
Bisacodyl is a stimulant laxative. That means it doesn’t soften stool like magnesium citrate or draw water into the colon like polyethylene glycol. Instead, it directly irritates the lining of the colon. This irritation triggers stronger muscle contractions, pushing stool out faster. Think of it like tapping your foot to get a stalled elevator moving. It’s not fixing the elevator-it’s giving it a jolt.
It’s available as tablets, suppositories, or even enemas. Most people with IBS use the oral tablets because they’re easier to control. The suppository version kicks in even faster-sometimes in under an hour-but it’s messier and harder to use regularly.
What makes bisacodyl different from other laxatives is its targeted action. It doesn’t affect the small intestine or stomach. It works almost entirely in the lower colon. That’s why it’s preferred for IBS-C over bulk-forming laxatives that can cause bloating and gas-common triggers for IBS flare-ups.
Why People with IBS-C Turn to Bisacodyl
IBS-C affects about 1 in 5 people with IBS. The main problem? Infrequent bowel movements-sometimes only once or twice a week-and hard, lumpy stools. Fiber helps, but not everyone can tolerate it. Some people get worse bloating. Others just don’t see results. That’s where bisacodyl steps in.
A 2023 review in the Journal of Neurogastroenterology and Motility found that over 60% of IBS-C patients who tried bisacodyl reported improved stool frequency and reduced straining within the first week. Not everyone, but enough that it’s still one of the most commonly prescribed laxatives for this subtype.
It’s not magic. It doesn’t reduce abdominal pain or bloating. In fact, if you take too much, it can make those symptoms worse. But for the simple goal of having a bowel movement when you haven’t had one in days? Bisacodyl often delivers.
When Bisacodyl Can Make IBS Worse
Here’s the catch: bisacodyl isn’t safe for daily use. Your colon starts to rely on it. Over time, the natural muscle contractions weaken. You need higher doses just to get the same result. That’s called laxative dependence-and it’s a real risk for people with chronic constipation.
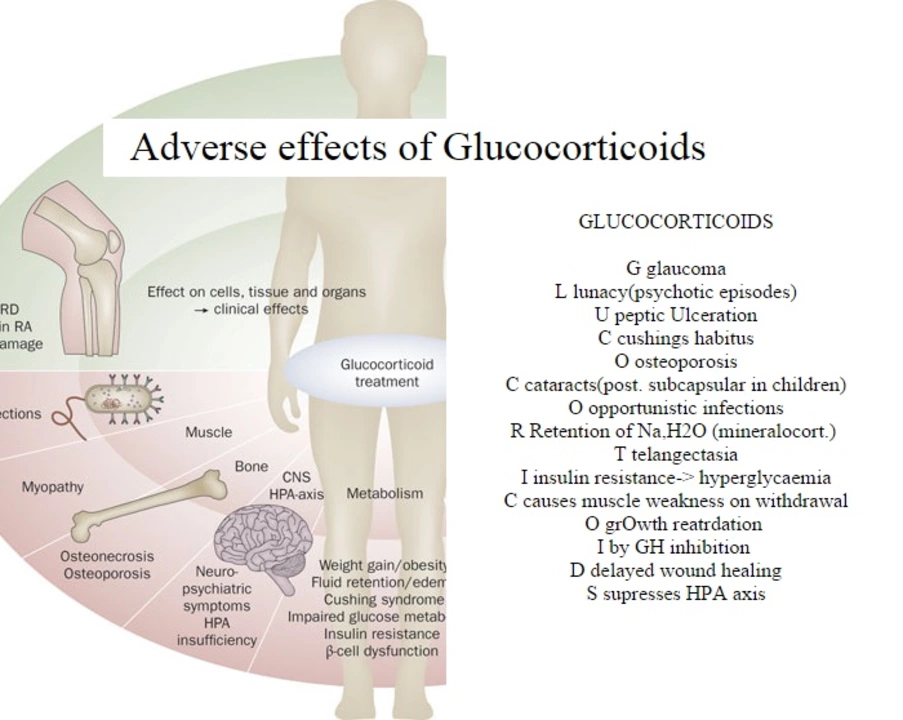
Studies show that using stimulant laxatives like bisacodyl for more than two weeks in a row increases the chance of developing electrolyte imbalances, especially low potassium. That can lead to muscle cramps, fatigue, and even irregular heartbeat. People with IBS are already prone to dehydration from avoiding fluids due to fear of bloating. Adding bisacodyl without drinking enough water makes that worse.
Another problem? It doesn’t fix the root cause. IBS-C is often tied to slow gut motility, altered nerve signaling, or even gut microbiome changes. Bisacodyl just forces movement. It doesn’t retrain your colon. That’s why doctors recommend it as a short-term tool, not a long-term solution.
How to Use Bisacodyl Safely with IBS
If your doctor says bisacodyl is right for you, here’s how to use it without causing more harm:
- Start low. Take one 5mg tablet at night. Don’t double up unless instructed.
- Wait 24-48 hours. Don’t take another dose unless you haven’t had a bowel movement after two days.
- Drink water. At least 8 ounces with the tablet, and aim for 2 liters total that day.
- Don’t use daily. Limit use to no more than 3-4 times a week, and never for longer than two weeks straight without checking in with your doctor.
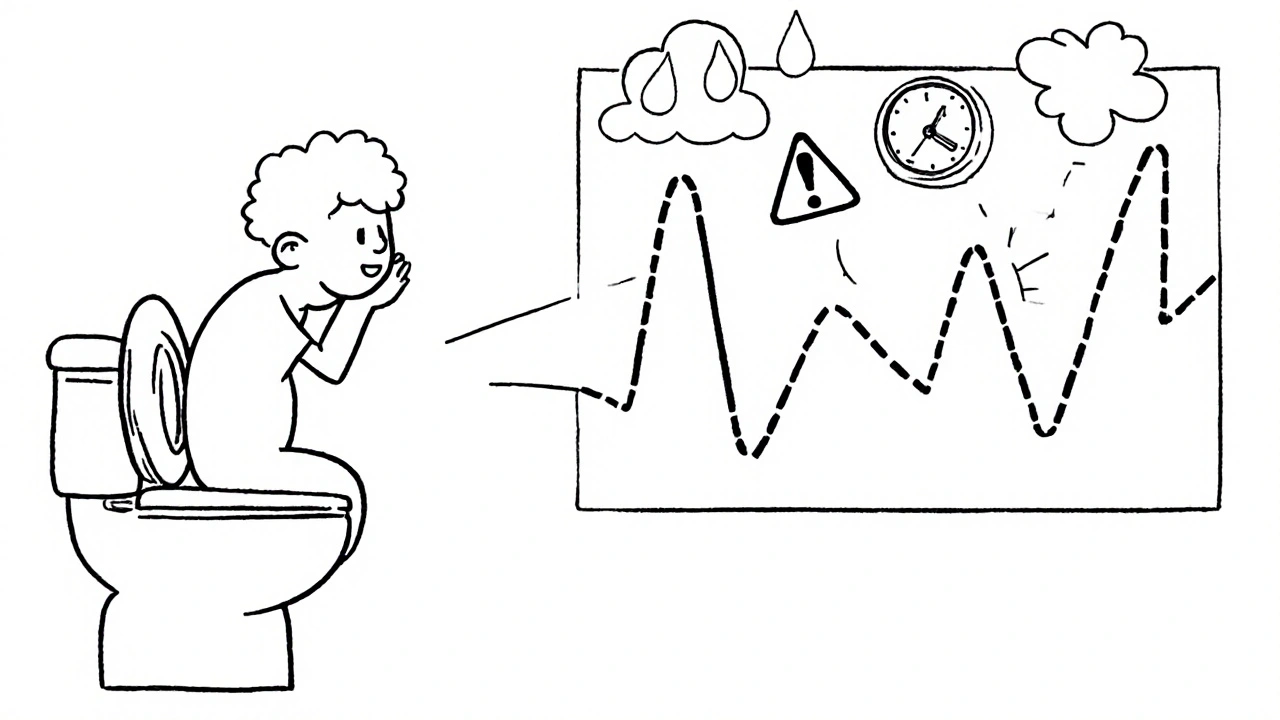
- Track your symptoms. Keep a simple log: date, dose, time of bowel movement, pain level, bloating. This helps you and your doctor spot patterns.
Some people find that using bisacodyl once every 5-7 days keeps things regular without triggering dependence. Others need it more often. The key is to be intentional, not reactive.
Alternatives to Bisacodyl for IBS-C
There are other options that might work better-or at least with fewer side effects:
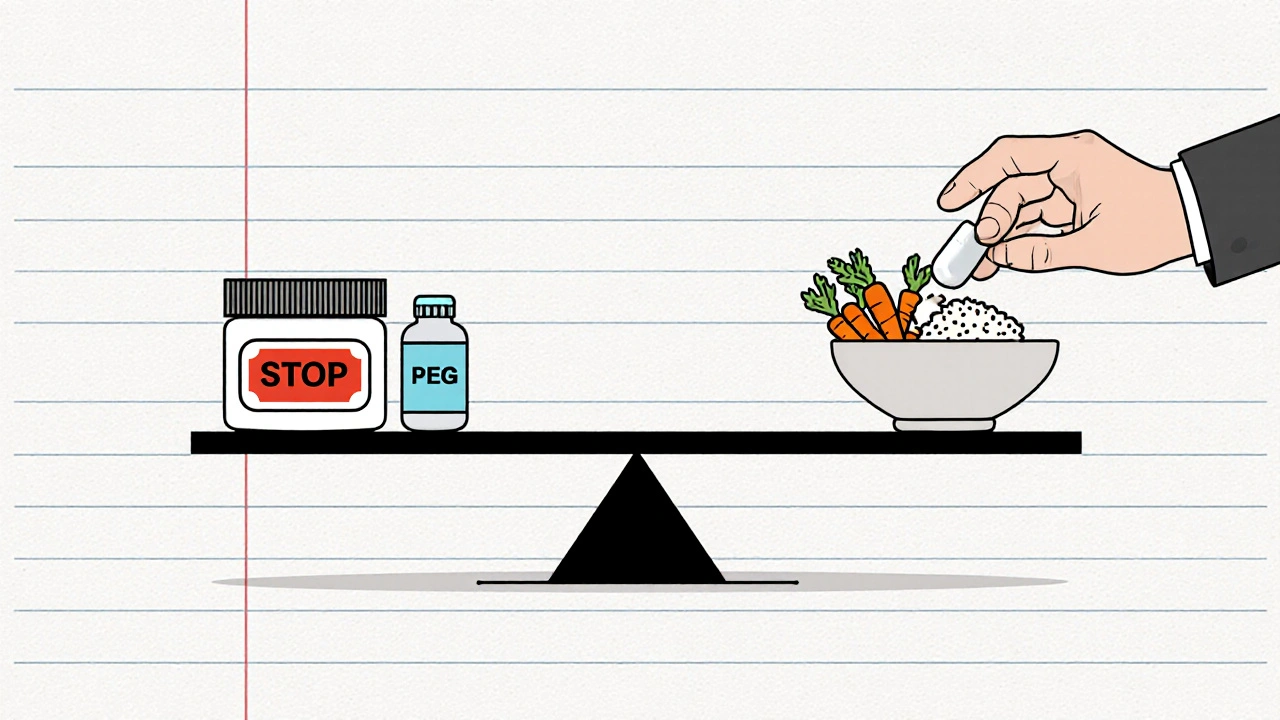
- Polyethylene glycol (PEG 3350): An osmotic laxative that pulls water into the colon. It’s gentler than bisacodyl and safe for daily use. Studies show it improves stool consistency without increasing pain.
- Linaclotide (Linzess): A prescription medication specifically approved for IBS-C. It works by increasing fluid secretion in the gut and reducing pain signals. More expensive, but often more effective long-term.
- Prucalopride (Resolor): A newer prokinetic drug that stimulates natural bowel contractions. Used in Europe and Canada, it’s not yet FDA-approved for IBS-C in the U.S., but sometimes prescribed off-label.
- Dietary changes: Low-FODMAP diet, increased soluble fiber (like psyllium), and consistent meal timing can improve motility without drugs.
Many people with IBS-C find that combining PEG with occasional bisacodyl gives them the best balance-regularity without dependency.
Who Should Avoid Bisacodyl Completely
Bisacodyl isn’t safe for everyone. Avoid it if you have:
- Intestinal blockage or severe abdominal pain (could be appendicitis or another emergency)
- Dehydration or kidney disease
- History of bowel surgery or inflammatory bowel disease (like Crohn’s or ulcerative colitis)
- Allergy to bisacodyl or other stimulant laxatives
- Pregnancy (unless approved by your OB-GYN-some studies suggest it’s low risk, but caution is advised)
If you’re unsure, talk to your doctor before taking it. Self-medicating with over-the-counter laxatives is common among IBS patients-but it’s also one of the most frequent reasons people end up in the ER with electrolyte issues or bowel damage.
The Bottom Line: Bisacodyl as a Tool, Not a Crutch
Bisacodyl can be a lifesaver for someone with IBS-C who hasn’t had a bowel movement in a week. But it’s not a long-term fix. Think of it like a fire extinguisher-you don’t live with it on all the time. You keep it handy for emergencies.
The goal isn’t to eliminate all constipation. It’s to reduce the stress and discomfort that comes with it. For many, that means using bisacodyl sparingly, pairing it with lifestyle changes, and knowing when to try something else.
If you’ve been relying on bisacodyl every few days for months, it’s time to talk to a gastroenterologist. There are better, safer ways to retrain your gut. But if you need it once a month to feel normal? That’s okay. Just make sure you’re not using it because you’re scared to stop.
Can bisacodyl cause dependency in IBS patients?
Yes. Regular use of bisacodyl-especially daily or several times a week for more than two weeks-can lead to dependency. Your colon may start to lose its natural ability to contract without stimulation. This is called laxative-induced colonic inertia. It’s reversible, but only if you stop using the drug and work with a doctor to retrain your bowel habits.
Is bisacodyl safe for long-term IBS management?
No. Bisacodyl is meant for short-term relief, not daily use. Long-term use increases the risk of electrolyte imbalances, dehydration, and reduced bowel function. For ongoing IBS-C symptoms, doctors recommend alternatives like polyethylene glycol, linaclotide, or dietary changes that address the root cause instead of just forcing movement.
Does bisacodyl help with IBS pain and bloating?
No. Bisacodyl only helps with constipation by stimulating bowel movements. It does not reduce abdominal pain, bloating, or gas. In fact, if you take too much, it can worsen cramping and discomfort. People with IBS who struggle with pain should focus on other treatments, like low-FODMAP diets, peppermint oil, or medications like linaclotide that target both motility and pain.
How quickly does bisacodyl work for IBS-C?
Oral bisacodyl tablets usually work within 6 to 12 hours. Suppositories can work in as little as 15 to 60 minutes. That’s why many IBS-C patients take it at night-to have a bowel movement by morning. Timing matters. Taking it too early in the day can lead to inconvenient urgency.
Can I take bisacodyl with other IBS medications?
It depends. Bisacodyl can be used with osmotic laxatives like PEG or fiber supplements like psyllium. But avoid combining it with other stimulant laxatives (like senna) or diuretics, as this increases the risk of dehydration and electrolyte loss. Always check with your doctor before mixing medications, especially if you’re taking prescription drugs like linaclotide or antidepressants for IBS.
What to Do Next
If you’re using bisacodyl regularly and want to cut back, start by tracking your bowel habits for two weeks. Note what you eat, how much water you drink, and when you take the medication. Then schedule a visit with a GI specialist. Bring your log. Ask about alternatives. You might be surprised how much improvement comes from small, consistent changes-not just stronger laxatives.







12 Comments