When your doctor prescribes a respiratory combination inhaler for asthma or COPD, you might assume that switching to a generic version is just like swapping one pill for another. But it’s not. These inhalers aren’t just about the chemicals inside-they’re about the device you use to get them into your lungs. And that device makes all the difference.
Why Generic Inhalers Aren’t Like Generic Pills
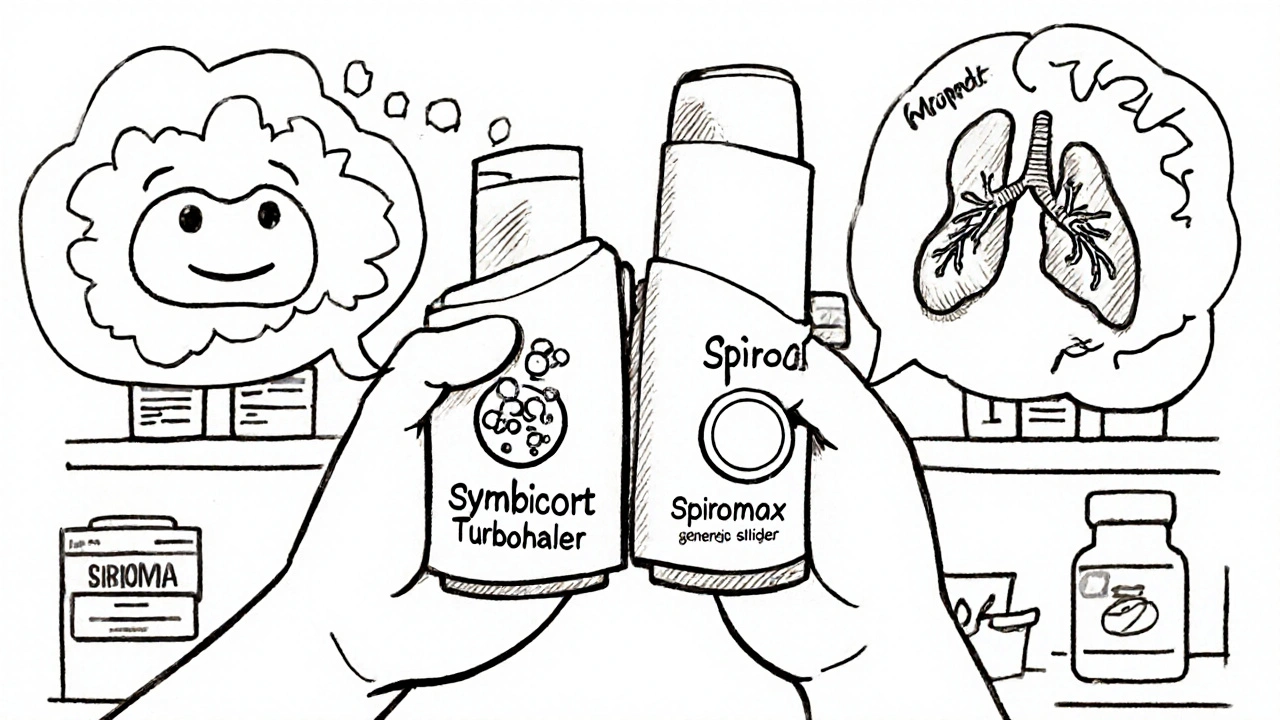
Most generic medications are chemically identical to their brand-name counterparts. Take ibuprofen: whether you buy Advil or a store brand, the active ingredient is the same, and your body processes it the same way. But with combination inhalers, the story changes. These devices deliver two drugs-usually a corticosteroid to reduce inflammation and a long-acting beta agonist to open airways-in one unit. The brand-name versions, like Symbicort Turbohaler or Advair Diskus, have been designed over years to ensure the medicine is released at the right speed, in the right amount, and reaches the right part of your lungs. Generic versions may contain the same drugs, but they often come in different devices. And that’s where things go wrong. A 2020 study found that 76% of patients switched from a Turbuhaler to a Spiromax without training used the device incorrectly. That’s not because they were careless. It’s because the two devices work differently. Turbuhaler requires a twist to load a dose. Spiromax uses a side slider. One needs a slow, deep breath. The other needs a sharp, forceful inhale. Get it wrong, and you’re not getting your medicine.The Device Is Part of the Medicine
The U.S. Food and Drug Administration (FDA) says generic inhalers are safe to substitute without extra training. But real-world evidence tells a different story. In the UK, the National Institute for Health and Care Excellence (NICE) explicitly warns against automatic substitution. Why? Because switching inhalers without proper instruction has been linked to worsening asthma control. A 2021 study published in the Journal of Aerosol Medicine and Pulmonary Drug Delivery showed that patients switched from Symbicort Turbohaler to the generic Spiromax without training had a 22% increase in asthma attacks within six months. Those who got proper instruction? No increase. The difference wasn’t the drug. It was the device. Even the European Medicines Agency (EMA), which regulates medicines across 30+ countries, requires proof that a generic inhaler delivers the same amount of medicine to the lungs as the original. That’s not just about chemical equivalence-it’s about how the device works. If the inhaler doesn’t disperse the powder the same way, or if the timing of the puff doesn’t match your breathing, the medicine won’t reach where it needs to go.What Happens When You’re Switched Without Warning
Many patients don’t even know they’ve been switched. Pharmacists, under pressure to cut costs, often substitute without telling the patient. One Reddit user wrote: “I didn’t realize I needed to breathe in harder. My asthma got so bad I ended up in hospital.” That story isn’t rare. A 2022 survey by Asthma UK found that 57% of patients felt confused after being switched to a different inhaler. Of those, 32% ended up in the emergency room within three months. On Drugs.com, Symbicort Turbohaler has a 6.2/10 rating from over 1,000 reviews. The generic Spiromax? 4.8/10 from 327 reviews. Common complaints: “Harder to use,” “Feels less effective,” “I don’t know how to use it.” Meanwhile, patients who received hands-on training from their pharmacist or doctor had an 89% success rate using the new device. The difference? Not the medicine. The instruction.
How Healthcare Providers Are Failing Patients
Doctors and pharmacists are stretched thin. A 2022 survey by the American Pharmacists Association found that only 28% of community pharmacies consistently offer device-specific training when substituting inhalers. Time is the biggest barrier-76% of pharmacists said they just don’t have it. But training isn’t complicated. The American Association for Respiratory Care recommends the “teach-back” method: show the patient how to use the device, then ask them to do it themselves. If they can’t do it right the first time, you show them again. That simple step increases correct technique from 35% to 82%. In Germany, pharmacists are legally required to give 15 minutes of in-person counseling for first-time inhaler users. In the U.S.? No such rule. The result? A 37% higher risk of improper use and treatment failure when substitution happens without consultation, according to the American Thoracic Society.Global Differences in Policy
Countries handle this differently-and the results show it. Norway has a 62% generic substitution rate for respiratory inhalers. France? Just 22%. Why? Because French guidelines require doctors to prescribe by brand name. That’s not about protecting profits. It’s about protecting patients. The Global Initiative for Asthma (GINA) updated its 2023 guidelines to say this clearly: “While cost considerations are important, device familiarity and correct technique should be prioritized over generic substitution.” That’s a big shift. It means even organizations focused on lowering costs now admit that switching devices can be dangerous. The FDA approved 17 generic inhalers between 2019 and 2023. The EMA approved only 8-and only after requiring clinical studies proving they worked the same way. The U.S. focuses on chemical equivalence. Europe focuses on real-world delivery. Which approach keeps patients safer?
What You Can Do to Stay Safe
If you’re on a combination inhaler, here’s what you need to do:- Ask your doctor: “Is this inhaler prescribed by brand name, or can it be substituted?”
- Ask your pharmacist: “Is this the same device as before? If not, can you show me how to use it?”
- Watch your symptoms: If you feel worse after a switch-more wheezing, more rescue inhaler use, more nighttime symptoms-don’t ignore it. Call your doctor.
- Request a demonstration: Even if you’ve used an inhaler for years, a new device can feel totally different. Ask for a practice session.
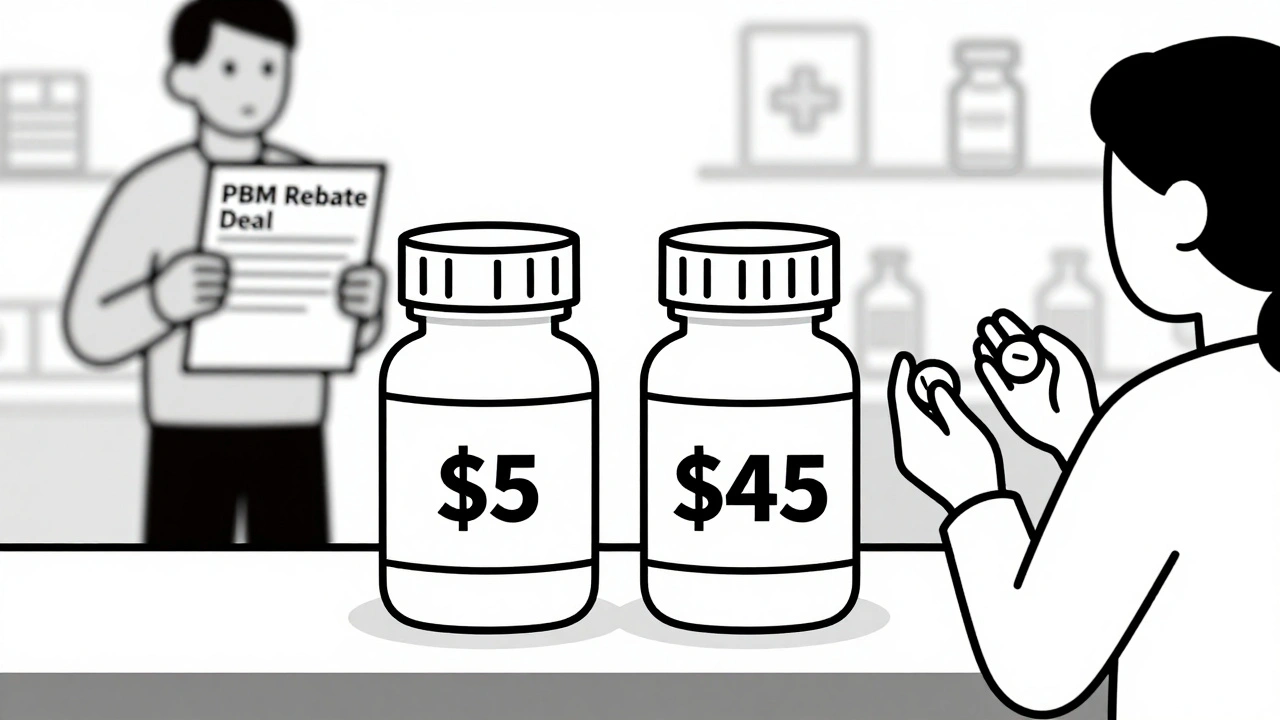
The Bigger Picture: Cost vs. Safety
Generic inhalers save money-on paper. The global market for respiratory inhalers was worth $14.7 billion in 2022. Generic versions make up about 18% of that. But the hidden cost? Emergency visits, hospital stays, missed work. A 2023 report estimated that inappropriate substitution costs U.S. healthcare systems $1.2 billion a year. That’s more than the savings from switching to cheaper inhalers. And it’s not just about money. It’s about quality of life. One patient told a reporter: “I used to run with my kids. Now I can’t walk to the mailbox without stopping to catch my breath.” That’s not a generic problem. That’s a system problem. New technologies are helping. Smart inhalers with sensors that track how you use them-like Propeller Health-are showing a 33% drop in asthma attacks when they give real-time feedback. But those aren’t widely available yet. Until then, the safest thing you can do is know your device and use it correctly.What’s Next?
By 2027, nearly half of all respiratory combination inhalers will face generic competition. That means more switches, more confusion, more risk-if nothing changes. The FDA is now requiring more clinical studies to prove therapeutic equivalence for inhalers. That’s a step forward. But real change will only happen when doctors, pharmacists, and patients all understand: this isn’t just a pill swap. It’s a device swap. And that requires training, awareness, and communication. If you’re on a combination inhaler, don’t wait for a crisis to ask questions. Ask now. Make sure you know how to use it. And if you’re switched without warning, speak up. Your lungs can’t afford a mistake.Can I switch my asthma inhaler to a generic version without talking to my doctor?
No, you shouldn’t. Generic combination inhalers often use different devices than the brand-name version, and using them incorrectly can reduce the medicine’s effectiveness or cause worsening symptoms. Always talk to your doctor or pharmacist before switching. They should show you how to use the new device and confirm you can do it right.
Why do some generic inhalers cost less but feel less effective?
They may contain the same drugs, but the device that delivers them is different. Some generics use dry powder inhalers that require a forceful breath, while others use metered-dose inhalers that need precise timing. If your technique doesn’t match the new device, you’re not getting the full dose. That’s not the drug failing-it’s the mismatch between you and the device.
Are all generic inhalers the same?
No. Two generics for the same drug combination can use completely different devices. For example, one might be a Turbuhaler-style device, while another is a Spiromax. Even if both contain budesonide and formoterol, the way you activate them, the force of breath needed, and how the powder disperses can vary. Always check the device type, not just the drug name.
How can I tell if my inhaler has been switched?
Look at the device. Does it look different? Is the shape, color, or button mechanism changed? Check the packaging-it should list the manufacturer and device type. If you’re unsure, ask your pharmacist: “Is this the same device I’ve been using?” Don’t rely on the drug name alone. The device matters just as much.
What should I do if I feel worse after switching inhalers?
Use your rescue inhaler if you have one, and contact your doctor right away. Keep a log of your symptoms: how often you’re using your rescue inhaler, whether you’re waking up at night, or if you’re having trouble with daily activities. Bring this info to your appointment. You may need to switch back or get proper training on the new device.
Is there a way to make sure I’m using my inhaler correctly?
Yes. Ask your doctor or pharmacist to demonstrate the correct technique, then ask you to show them how you do it-that’s called the “teach-back” method. Studies show this increases correct use from 35% to 82%. You can also find video tutorials from reputable sources like the American Lung Association or GINA. Practice in front of a mirror. If you’re still unsure, schedule a follow-up.
If you’re managing asthma or COPD, your inhaler is your lifeline. Don’t let a switch to a cheaper version become a risk to your health. Ask questions. Demand training. Know your device. Your lungs depend on it.





15 Comments