Decongestant Safety Risk Calculator
This calculator helps you understand the safety risks of decongestants based on your heart health status. Decongestants can dangerously affect blood pressure and heart function, especially for people with existing heart conditions.
If you have heart disease or high blood pressure, taking a common cold medicine might be riskier than you think. Decongestants like pseudoephedrine and phenylephrine are in almost every over-the-counter cold and flu remedy. They promise quick relief from a stuffy nose-but for people with heart conditions, that relief can come at a dangerous cost.
How Decongestants Work (and Why That’s a Problem for Your Heart)
Decongestants shrink swollen blood vessels in your nose to open up your airways. That’s why they work so fast. But here’s the catch: they don’t just shrink vessels in your nose. They tighten blood vessels all over your body. That’s how they raise your blood pressure.
These medications are alpha-adrenergic agonists. That’s a fancy way of saying they mimic the effects of adrenaline. Your heart starts beating harder and faster. Your arteries get tighter. For someone with a healthy heart, this might cause only a small, temporary spike in blood pressure. But for someone with heart disease, uncontrolled hypertension, or a history of stroke or heart attack, this stress can trigger serious problems-like irregular heart rhythms, chest pain, or even a heart attack.
Studies confirm this. A 2005 meta-analysis found that pseudoephedrine causes a small but measurable increase in systolic blood pressure-especially with higher doses or immediate-release forms. Even a 5-year-old girl developed high blood pressure after standard doses of phenylephrine. Her pressure returned to normal only after stopping the medication. That’s not a rare case. It’s a warning sign.
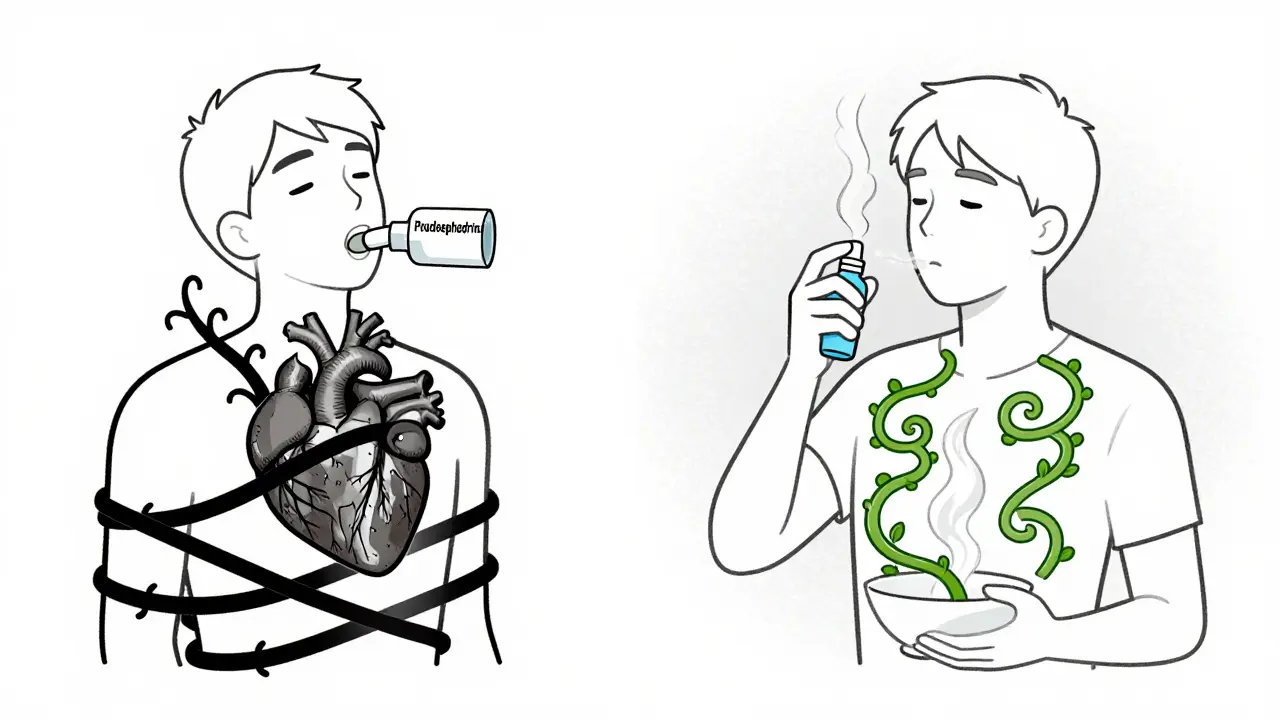
Oral vs. Nasal: Which Is Riskier?
Not all decongestants are the same. Oral ones-like Sudafed (pseudoephedrine) and newer phenylephrine products-enter your bloodstream and affect your whole body. That’s why they’re more dangerous for people with heart conditions.
Topical nasal sprays like Afrin (oxymetazoline) or naphazoline seem safer because they’re applied locally. But they’re not risk-free. A study of 100 patients showed their heart rate increased significantly after just a week of use. And in one documented case, a 40-year-old man developed life-threatening heart failure after using too much naphazoline spray. He didn’t take an overdose by accident-he was following the label. But the label doesn’t warn enough about what happens when these sprays are used daily for days on end.
Even if you’re careful with the dose, the effect builds up. Your body doesn’t reset quickly. That’s why doctors say: if you have heart disease, avoid these sprays too.
Who’s at the Highest Risk?
It’s not just about having high blood pressure. Certain heart conditions make decongestants especially dangerous:
- Uncontrolled hypertension - Your blood pressure is already too high. Decongestants push it higher, sometimes into the danger zone.
- Heart failure - Your heart is already struggling to pump. Decongestants make it work harder, which can cause fluid to build up in your lungs.
- Arrhythmias - Irregular heartbeats can turn into dangerous rhythms like ventricular tachycardia when decongestants stimulate the heart.
- Prinzmetal angina - This rare condition causes sudden coronary artery spasms. Decongestants can trigger those spasms, cutting off blood flow to the heart.
The American Heart Association says people with any of these conditions should avoid oral decongestants entirely. The Mayo Clinic and Harvard Health say the same. Even if your blood pressure is "controlled" with medication, you still need to talk to your doctor before using any decongestant.
What About Cold and Flu? Isn’t It Just a Cold?
Here’s something many people don’t realize: having a cold or the flu already puts stress on your heart. Your body fights the infection by raising your heart rate and causing inflammation. Your heart is already working harder.
Add a decongestant on top of that, and you’re stacking risks. A 2017 study of nearly 10,000 heart attack patients found that those who took NSAIDs (like ibuprofen) while sick were more than three times as likely to have another heart attack within a week. Decongestants aren’t NSAIDs, but they do the same thing-they add extra strain when your body is already under pressure.
It’s not about being weak. It’s about biology. Your heart isn’t designed to handle multiple stressors at once. And decongestants are one of the most common hidden stressors.
What Should You Use Instead?
You don’t need decongestants to feel better. There are safer ways to manage congestion:
- Saline nasal sprays - These just flush out mucus and irritants. No chemicals. No blood pressure spikes.
- Steam inhalation or humidifiers - Moist air helps loosen congestion naturally.
- Guaifenesin (Mucinex) - This thins mucus so you can clear it easier. It doesn’t constrict blood vessels.
- Rest and hydration - Your body heals better when it’s not fighting dehydration or exhaustion.
Some people think, "I’ll just use it once." But even one dose can be enough to trigger a problem in someone with a sensitive heart. And if you’re already taking blood pressure meds, decongestants can interfere with their effectiveness.
What About Behind-the-Counter Decongestants?
Pseudoephedrine is kept behind the pharmacy counter in the U.S. and Australia. That’s not just for drug control-it’s for safety. Pharmacists are trained to ask questions: "Do you have high blood pressure? Heart disease? Trouble urinating?" They’re your last line of defense.
If you’re buying pseudoephedrine, the pharmacist should stop you if you have heart disease. If they don’t, speak up. Say: "I have heart issues. Is this safe?" Don’t assume they know your full medical history. Many people don’t tell them.
And never buy decongestants online without checking the label. Some websites sell products without proper warnings. That’s how people end up in emergency rooms.
Reading Labels Isn’t Enough-You Need to Understand Them
Most decongestant bottles say: "Do not use if you have high blood pressure or heart disease." But people skim. They think, "I’m fine, I take medicine for it." Or, "It’s just one tablet." But here’s the truth: the label isn’t there to scare you. It’s there to save your life.
Look for these ingredients: pseudoephedrine, phenylephrine, ephedrine, oxymetazoline, naphazoline. If you see any of them, and you have heart disease or high blood pressure, don’t take it.
And watch out for combination products. Cold remedies often mix decongestants with pain relievers, antihistamines, or cough suppressants. You might think you’re getting one thing-but you’re getting a heart-stressing cocktail.
The Bottom Line
Decongestants give fast relief. But they don’t cure anything. They just mask symptoms. For someone with heart disease, that mask can hide a ticking time bomb.
There’s no safe dose of pseudoephedrine if you have uncontrolled high blood pressure. There’s no safe duration of nasal spray use if you have heart failure. And there’s no excuse to ignore the warnings on the bottle.
If you have heart disease or hypertension, skip the decongestants. Use saline sprays. Use steam. Rest. Drink water. Talk to your doctor before taking anything new-even if it’s "just a cold." Your heart doesn’t need a boost. It needs protection.
Can I take pseudoephedrine if my blood pressure is controlled?
Even if your blood pressure is controlled with medication, pseudoephedrine can still interfere with your treatment and raise your pressure beyond safe levels. The American Heart Association and Mayo Clinic recommend avoiding it entirely if you have heart disease. Always check with your doctor first-even if you think your condition is stable.
Are nasal sprays safer than pills for people with heart disease?
Not necessarily. While nasal sprays like oxymetazoline act more locally, they still enter the bloodstream, especially with frequent or prolonged use. Studies show they can increase heart rate and, in rare cases, trigger heart failure or dangerous spikes in blood pressure. The risk is lower than with oral decongestants, but it’s not zero. Avoid them if you have heart disease.
What are the signs that a decongestant is affecting my heart?
Watch for rapid or irregular heartbeat, chest tightness, dizziness, severe headache, or sudden shortness of breath. These aren’t normal side effects-they’re warning signs. Stop the medication immediately and seek medical help if you experience any of these.
Can decongestants cause a heart attack?
Yes. While rare, there are documented cases where decongestants triggered heart attacks in people with underlying heart disease. The vasoconstriction they cause can reduce blood flow to the heart muscle, especially in people with narrowed arteries. This risk is higher during illness, when your body is already under stress.
Is phenylephrine safer than pseudoephedrine?
No. Although phenylephrine is now the most common oral decongestant in the U.S. (replacing pseudoephedrine in many products), studies show it still raises blood pressure, especially in higher doses or with repeated use. It’s not safer for people with heart disease-it’s just less available behind the counter. Both should be avoided.
What should I do if I already took a decongestant and have heart disease?
Stop taking it immediately. Monitor your symptoms: check your pulse, blood pressure if you have a monitor, and watch for chest pain, dizziness, or trouble breathing. If you feel unwell, call your doctor or go to the nearest emergency room. Don’t wait. Even a single dose can be dangerous if you’re at risk.