By January 2026, millions of Americans are seeing their prescription bills drop-some by hundreds of dollars a year. That’s not magic. It’s policy. The Inflation Reduction Act finally started delivering real savings, and it’s changing how people pay for meds. But if you’re still confused about why your insulin costs $30 one month and $150 the next, you’re not alone. The system is messy. Coupons, generics, and prior authorizations aren’t just buzzwords-they’re tools, traps, and sometimes lifelines. Here’s how they actually work today-and what you can do to pay less.
Why Your Prescription Price Feels Random
Pharmaceutical pricing in the U.S. isn’t like buying groceries. There’s no sticker price. There’s the list price-the number you see on the manufacturer’s website. Then there’s the net price-the actual amount the pharmacy gets after rebates, discounts, and negotiations. And then there’s what you pay, which depends on your insurance, your pharmacy, and whether your PBM (pharmacy benefit manager) decided to steer you to a specific store. For example, a 30-day supply of metformin might be listed at $120. But after rebates, the net price could be $10. If your insurance has a $10 copay, you pay $10. But if you’re uninsured or your plan doesn’t cover it well, you might pay the full $120. That’s not a mistake. That’s how the system is built.Generics: The Silent Savings Engine
Generic drugs are the quiet heroes of affordable medicine. They’re chemically identical to brand-name drugs but cost 80-85% less. Yet, many people still reach for the name brand because they’re not sure generics work the same. They do. The FDA requires generics to meet the same standards for safety, strength, and effectiveness. A 2024 study in JAMA reviewed over 1,000 generic drugs and found no meaningful difference in outcomes compared to brand names. That includes drugs for high blood pressure, depression, and diabetes. But here’s the catch: not all generics are created equal. Some manufacturers make lower-quality versions. If you switch from one generic to another and feel different-dizziness, nausea, worse symptoms-talk to your pharmacist. You might need to stick with a specific brand of generic. Companies like Mark Cuban’s Cost-Plus Drugs is a direct-to-consumer pharmacy that sells generics at cost plus a flat $3 fee, often 30% cheaper than traditional pharmacies have proven you can buy real generics without the middlemen inflating prices.Coupons: Useful, But With Strings Attached
Pharmaceutical companies love coupons. You see them online, in mailers, on TV: “Save $50 on your Eliquis prescription.” Sounds great, right? It is-if you’re insured. But here’s the twist: these coupons often only work if you have private insurance. They’re designed to reduce your out-of-pocket cost so you’ll keep taking the expensive brand-name drug. That means your insurer pays more. And over time, that drives up premiums for everyone. Worse, coupons can’t be used with Medicare Part D or Medicaid. If you’re on Medicare, you’ll pay the full price unless you qualify for a low-income subsidy. And if you’re uninsured? Some coupons work, but only at certain pharmacies. Always ask: “Can I use this coupon without insurance?” If the answer is no, skip it. Better options? Use GoodRx is a free service that compares cash prices at nearby pharmacies and often finds lower rates than insurance copays. In 2025, GoodRx found that for 7 out of 10 top-selling drugs, the cash price without insurance was lower than the insurance copay.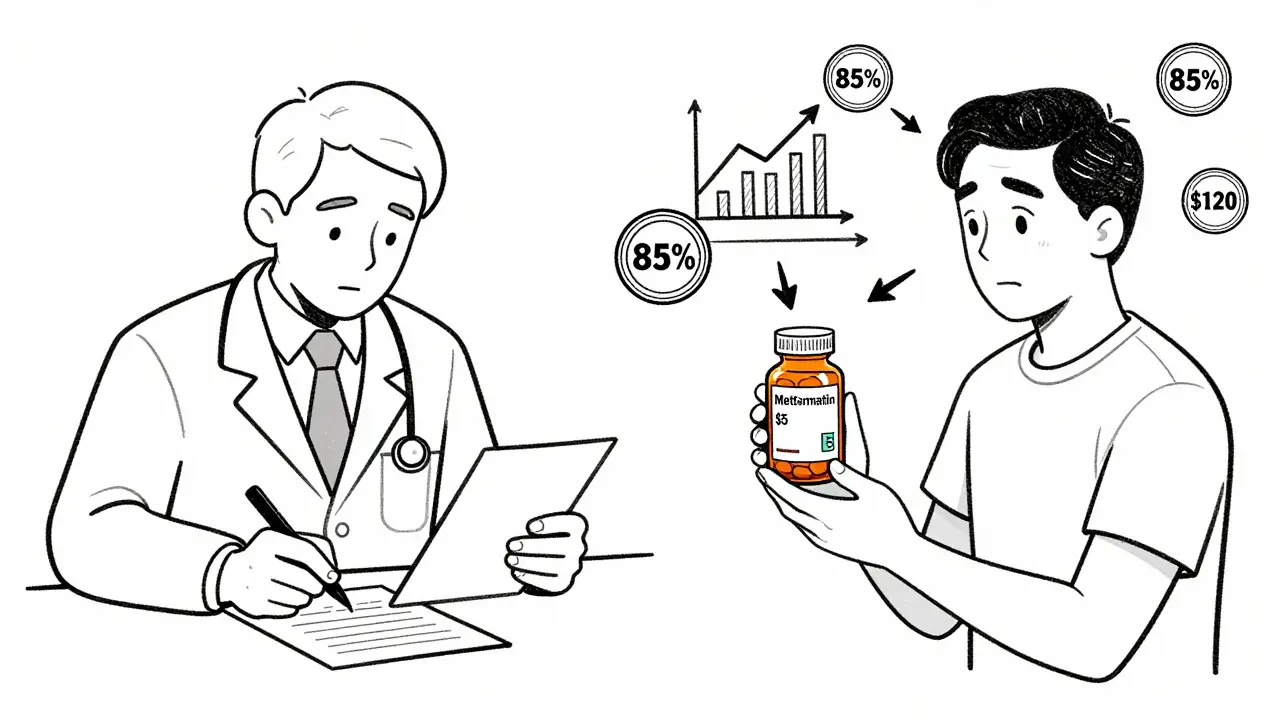
Prior Authorization: The Bureaucratic Hurdle
Prior authorization is when your insurance says, “Hold on. We need to approve this drug before you get it.” It’s meant to stop overuse of expensive meds. But in practice, it’s a delay tactic. Your doctor writes a prescription. The pharmacy sends a request to your insurer. The insurer asks for lab results, prior treatment records, or proof you tried cheaper alternatives first. It can take days. Or weeks. If you’re waiting for a life-saving drug like a GLP-1 for diabetes or a cancer treatment, that delay can be dangerous. A 2025 survey by the American Medical Association found that 92% of physicians reported prior authorization delays harmed patient care. And 83% said insurers often denied requests for drugs that were clearly medically necessary. What can you do? Ask your doctor to file the prior auth before you go to the pharmacy. Call your insurer and ask what they need. Write it down. Keep copies. If it’s denied, ask for a written explanation and file an appeal. Many denials get reversed on appeal.Medicare’s Big Shift in 2026
If you’re on Medicare, January 2026 is a turning point. For the first time, the government negotiated prices for 10 high-cost drugs-including insulin, blood thinners, and asthma inhalers. Those prices drop by 22% on average. You’ll pay less at the pharmacy counter. Plus, the $2,000 annual out-of-pocket cap for Medicare Part D is now in effect. No more climbing back up the “donut hole.” Once you hit $2,000, your drug costs are covered for the rest of the year. Nearly 19 million seniors will save an average of $400 per year. That’s not a small thing. It means people can afford to take their meds consistently. And that reduces hospital visits, ER trips, and long-term complications. But here’s the gap: these savings only apply to Medicare. If you’re under 65 and on private insurance, you’re still stuck with the old system. That’s why states are stepping in.State-Level Solutions Are Picking Up Speed
Nine states now have Prescription Drug Affordability Boards. These are government panels that review drug prices and set upper limits on what insurers and state programs can pay. Minnesota is leading the pack. They’ve tied their price caps directly to the new Medicare negotiated prices. If Medicare pays $30 for a drug, Minnesota caps private insurers at $35. That’s huge. California, Colorado, and Maine have similar rules. In 2025, Vermont passed a law requiring drugmakers to justify price hikes over 10% in a year. If they can’t, the state can block the increase. These aren’t perfect. Drug companies are suing. But they’re forcing transparency. And they’re giving people real relief.
What You Can Do Right Now
You don’t have to wait for policy to fix this. Here’s your action plan:- Ask for generics-every time. Even if your doctor says “brand only,” ask if there’s a generic equivalent.
- Use GoodRx or SingleCare-compare cash prices before you pay. Sometimes it’s cheaper than insurance.
- Check for manufacturer assistance programs-many drugmakers offer free or low-cost meds to low-income patients. Go to NeedyMeds.org.
- Know your prior auth rights-if your drug is denied, file an appeal. Keep records. Call your insurer’s ombudsman.
- Don’t skip doses to save money-talk to your doctor. There’s almost always a cheaper option.
What’s Coming Next
The GENEROUS Model for Medicaid is launching in 2026. It’s designed to make sure Medicaid pays no more than what other countries pay for the same drugs. That could cut prices by 15-25% for millions of low-income Americans. Biosimilars-cheaper versions of biologic drugs like Humira and Enbrel-are finally hitting the market. In 2025, the first biosimilar to Humira saved patients up to 70%. More are coming. And if the April 2025 executive order moves forward, Medicare could start negotiating 30 drugs per year by 2027. That’s a big deal. It could save over $500 billion over the next decade. The system is still broken. But it’s not hopeless. Change is happening-slowly, messily, but undeniably. Your job? Stay informed. Ask questions. Push back. And never assume your price is fixed.Are generic drugs really as good as brand-name drugs?
Yes. The FDA requires generics to have the same active ingredients, dosage, strength, and effectiveness as brand-name drugs. Studies show no meaningful difference in outcomes. Some people notice minor differences in fillers or coatings, which can affect how the pill dissolves. If you feel different after switching, tell your pharmacist. You can often request a specific generic manufacturer.
Can I use a coupon with Medicare?
No. Pharmaceutical manufacturer coupons cannot be used with Medicare Part D or Medicaid. These coupons are designed to reduce your out-of-pocket cost when you have private insurance, but they’re not allowed under federal programs. If you’re on Medicare, use GoodRx or check if the drugmaker offers a patient assistance program.
Why does my drug cost so much more at one pharmacy than another?
Because pharmacies negotiate different prices with your insurance or PBM. Some pharmacies are owned by the same company that runs your insurance, and they may charge more to make up for rebates they don’t get. Independent pharmacies often have better cash prices. Always compare prices using GoodRx before you pay.
What’s the difference between a prior authorization and a step therapy?
Prior authorization is when your insurer requires approval before covering a drug. Step therapy is a specific type of prior auth where you must try cheaper drugs first before they’ll cover the one your doctor prescribed. For example, you might have to try two generic blood pressure pills before they’ll cover the brand-name one. Both can delay care, but step therapy is more common for chronic conditions.
Is there a limit to how much I’ll pay for prescriptions in 2026?
If you’re on Medicare Part D, yes. The out-of-pocket cap is $2,000 per year. Once you hit that, your plan covers 100% of your drug costs for the rest of the year. For private insurance, there’s no federal cap-but some states are starting to set their own limits. Check your state’s health department website.
Can I buy prescription drugs from Canada to save money?
Technically, it’s illegal under U.S. law to import prescription drugs from Canada or other countries. But in practice, the FDA doesn’t target individual consumers. Many people do it safely through licensed Canadian pharmacies. If you choose this route, only use pharmacies verified by the Canadian International Pharmacy Association (CIPA). Never buy from random websites-many sell fake or expired meds.








9 Comments