Vitamin A Safety Checker for Pregnancy
Check Your Vitamin A Intake
Calculate your total preformed vitamin A intake from supplements and diet during pregnancy. The safe daily limit is 10,000 IU. Exceeding this increases the risk of birth defects.
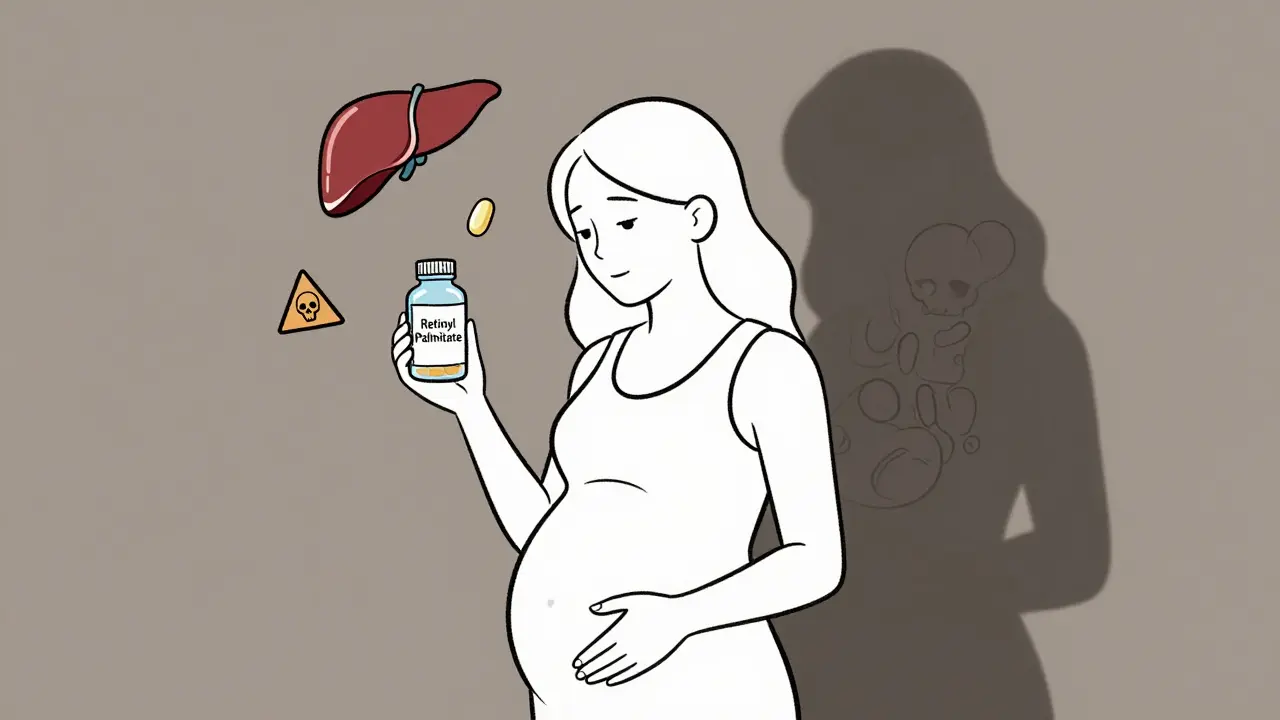
When you think of vitamin A, you probably picture glowing skin, healthy eyes, or a strong immune system. But what if that same nutrient, taken in the wrong form or dose during pregnancy, could cause serious birth defects? The truth is, retinoids and preformed vitamin A aren’t just harmless supplements-they’re powerful drugs with known, documented risks to unborn babies.
What Exactly Are Retinoids and Vitamin A?
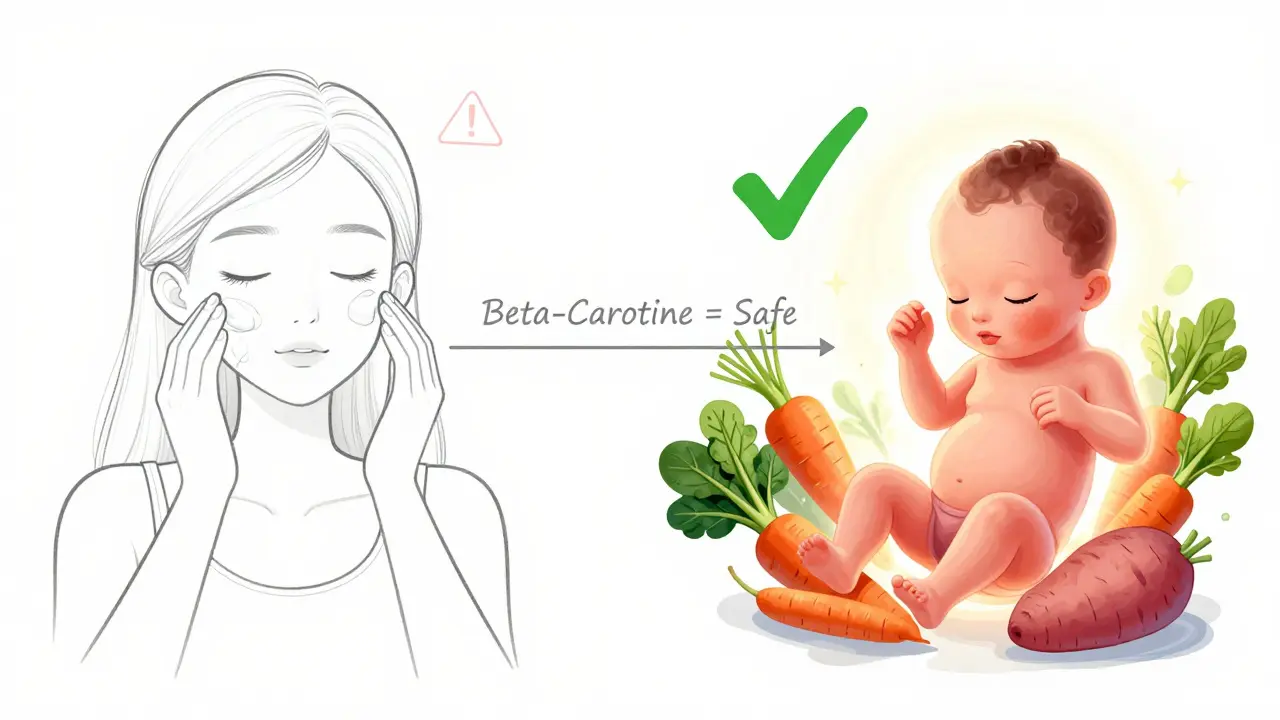
Vitamin A isn’t one thing. It’s a group of compounds, and not all of them are created equal. There’s preformed vitamin A-found in animal products like liver, fish oils, and dairy-and then there’s provitamin A carotenoids, like beta-carotene, found in carrots, sweet potatoes, and spinach. Your body turns beta-carotene into vitamin A only as needed. That’s why it’s safe. Preformed vitamin A, on the other hand, is stored in your liver and doesn’t get regulated the same way. Once it’s in, it stays. Retinoids are synthetic versions of vitamin A, made for medical use. The most well-known is isotretinoin (Accutane®), used for severe acne. Others include etretinate and acitretin. These aren’t supplements. They’re potent drugs designed to change how your skin cells behave. And they don’t just affect skin-they interfere with how embryos develop.When Does the Risk Start?
The danger isn’t there from day one of pregnancy. It’s focused on a narrow window: weeks 3 to 5 after conception. That’s when your baby’s heart, brain, eyes, ears, and jaw are forming. This is called organogenesis. During this time, even small amounts of excess retinoids can disrupt the signals that tell cells where to go and what to become. In 1953, scientist Sidney Q. Cohlan first proved this in rats. He gave pregnant rats massive doses of vitamin A-and their babies were born with missing eyes, cleft palates, and brains that didn’t close properly. Human studies later confirmed the same pattern. Babies exposed to high doses of retinoids during this window have a 20-35% chance of major birth defects. That’s 25 times higher than the baseline risk.How Dangerous Are Different Forms?
Not all vitamin A is equally risky. Here’s the breakdown:- Isotretinoin (Accutane®): The most dangerous. Just 0.5-1.0 mg per kg of body weight per day can cause defects. Even after stopping the drug, it takes weeks to clear from your system.
- Etretinate (Tigason®): Even worse. It stays in your body for up to 120 days. That means you need to avoid pregnancy for a full 3 years after your last dose.
- Acitretin: Still risky. It clears faster than etretinate, but you still need 2 years of contraception after stopping.
- Preformed vitamin A (retinol, retinyl palmitate): Dangerous above 10,000 IU per day. That’s less than you’d think. One 3-ounce serving of beef liver has 27,000 IU. A single supplement pill can hit 15,000 IU.
- Beta-carotene: Safe. Your body only converts what it needs. Even 180 mg per day (300,000 IU equivalent) shows no signs of harm in studies.
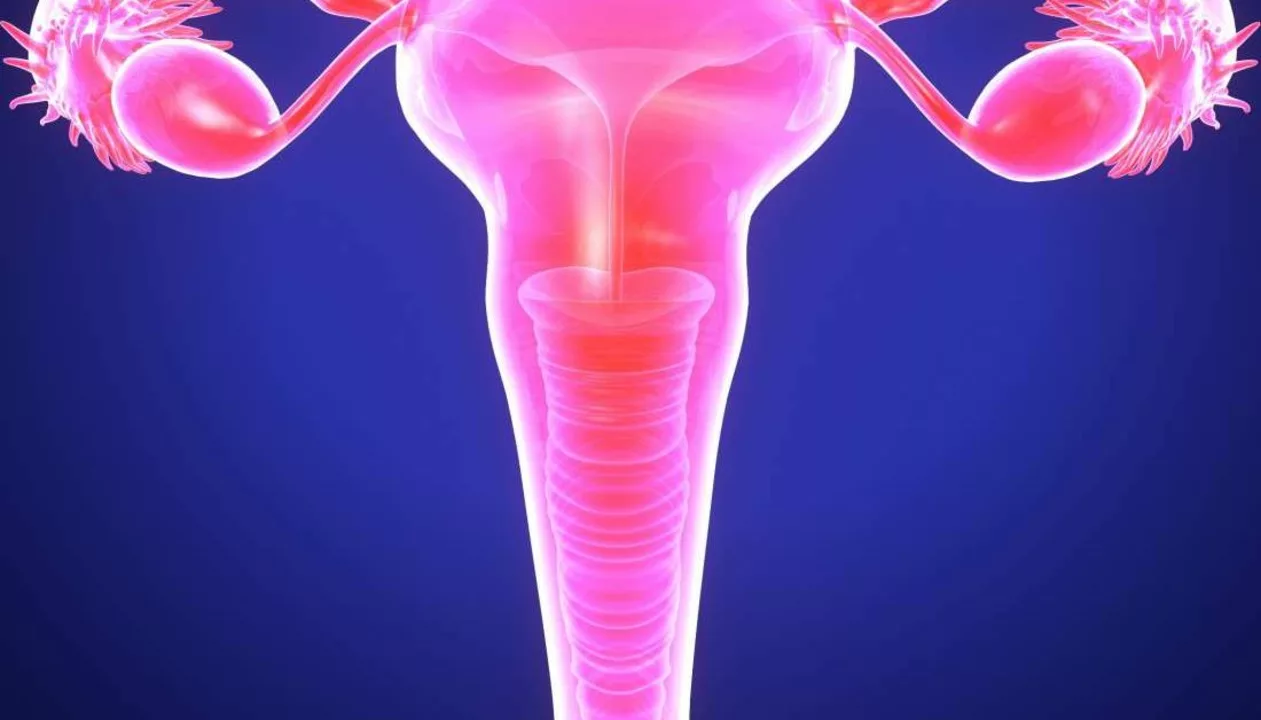
What Birth Defects Happen?
The defects aren’t random. They follow a pattern because retinoids mess with the same genes that control body layout-especially the Hox genes. Common outcomes include:- Cleft lip and palate
- Small or absent ears, hearing loss
- Heart defects (like ventricular septal defects)
- Brain malformations (exencephaly, microcephaly)
- Underdeveloped jaw (brachygnathia)
- Eye abnormalities (microphthalmia, coloboma)
Topical Retinoids: Are They Safe?
If you’re using tretinoin cream for acne or wrinkles, you might think you’re safe. And you probably are. Studies show that after applying standard doses of topical retinoids, blood levels of the drug stay below 0.5 ng/mL-too low to reach the embryo. The FDA still recommends caution during pregnancy, but the risk is minimal compared to oral forms. Still, some doctors advise switching to non-retinoid alternatives during pregnancy just to eliminate any uncertainty. Products with bakuchiol, azelaic acid, or niacinamide are popular replacements.What About Prenatal Vitamins?
Here’s where things get messy. Most prenatal vitamins contain preformed vitamin A-usually as retinyl palmitate. Consumer Reports found that, on average, they contain 2,565 IU per serving. That’s under the 10,000 IU danger zone. But some brands go higher. And if you’re also eating liver once a week or taking a separate vitamin A supplement, you could easily cross the line. The American College of Obstetricians and Gynecologists (ACOG) says: avoid daily supplements with more than 10,000 IU of preformed vitamin A. The World Health Organization agrees. But here’s the problem: many women don’t know the difference between beta-carotene and retinol. Labels don’t always make it clear. One study found that 45% of prenatal vitamins contain retinyl palmitate, and 73% of standalone vitamin A supplements are preformed.Real Stories, Real Consequences
On Reddit, a user named AcneWarrior2021 wrote in June 2023: “My dermatologist didn’t properly explain the pregnancy risks with Accutane-I got pregnant 3 weeks after my last dose and had to terminate due to confirmed risk of craniofacial defects.” On BabyCenter, HealthyMama2022 shared: “My OB warned me about liver and cod liver oil supplements during pregnancy-after researching, I switched to beta-carotene-only prenatal vitamins and felt much safer.” The National Birth Defects Prevention Network found that 15-20% of vitamin A-related birth defects happened in women who never took prescription retinoids. They just ate liver, took a high-dose supplement, or drank too much cod liver oil.
How Are Doctors Trying to Prevent This?
The FDA’s iPLEDGE program is the strictest drug safety system in the U.S. For isotretinoin, you must:- Have two negative pregnancy tests before starting
- Use two forms of birth control
- Attend monthly counseling
- Get a new prescription every month
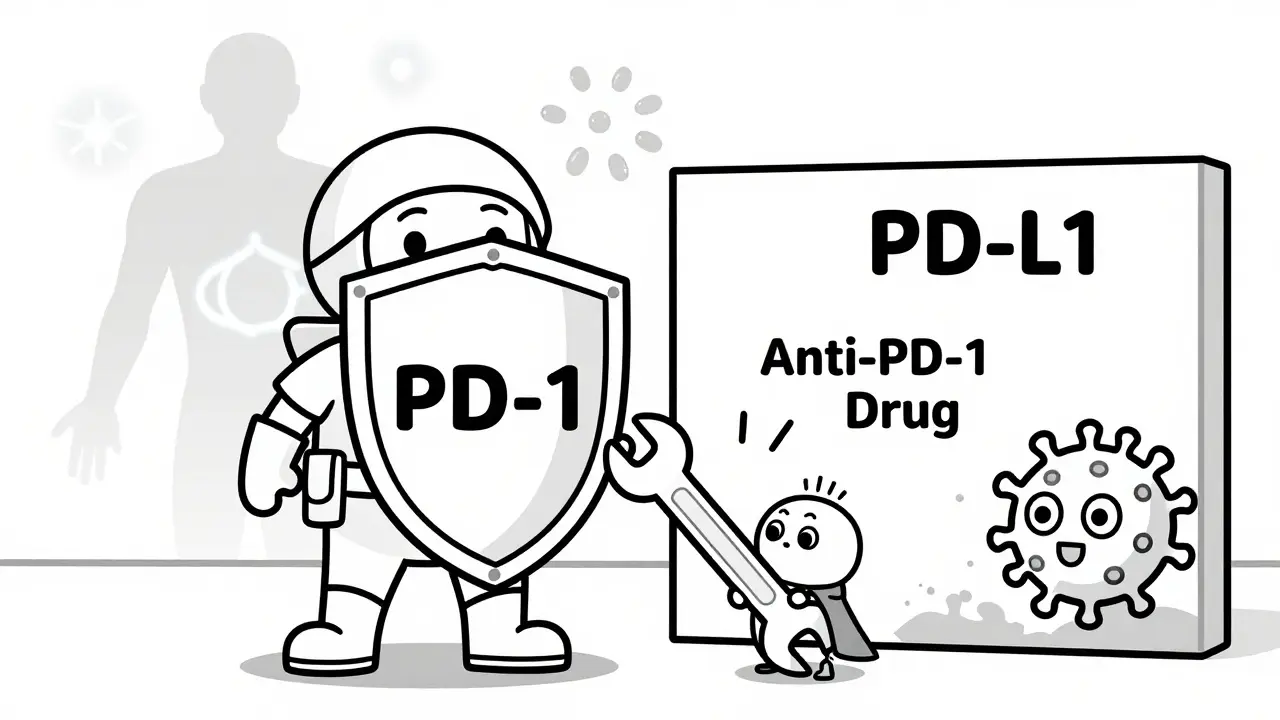
What’s Changing in 2026?
New research is trying to fix the problem at its source. LGD-1550, a new retinoid analog, is in Phase II trials. So far, it works as well as isotretinoin for acne-but doesn’t cause birth defects in animal studies. If it passes human trials, it could replace Accutane within the next 5 years. The Vitamin A Safety Consortium, funded by the NIH, is rolling out new patient education tools. Early results show a 32% improvement in how well women understand the risks. And the European Food Safety Authority just reaffirmed its 3,000 μg RAE (10,000 IU) upper limit for pregnant women. Meanwhile, the FDA is considering new rules to require clearer labeling on high-vitamin A foods like liver and supplements.What Should You Do?
If you’re pregnant or planning to be:- Check your prenatal vitamin. Look for “beta-carotene” as the only source of vitamin A. Avoid anything listing “retinol,” “retinyl palmitate,” or “retinyl acetate.”
- Stop eating liver, cod liver oil, or high-dose vitamin A supplements. Even one serving of liver can exceed your daily limit.
- If you’re on isotretinoin or any oral retinoid, use two forms of birth control. Don’t assume one method is enough.
- Wait at least one month after stopping isotretinoin before trying to conceive. For acitretin, wait two years. For etretinate, wait three.
- If you’re unsure, ask your doctor for a blood test to check your vitamin A levels. They’re not routinely done, but they can help if you’re worried.
Final Thought: Knowledge Is the Only Protection
Vitamin A is essential. But like many things, it’s a matter of dose and form. You can’t avoid it entirely-and you shouldn’t. But you can avoid the dangerous versions. The difference between a healthy baby and a preventable birth defect often comes down to one question: “Is this vitamin A from beta-carotene… or from retinol?” If you don’t know the answer, ask. Read the label. Talk to your doctor. Don’t assume it’s safe just because it’s labeled “natural” or “vitamin.”Can I take vitamin A while pregnant?
Yes-but only if it’s from beta-carotene, not preformed vitamin A. Avoid supplements or prenatal vitamins that contain retinol, retinyl palmitate, or retinyl acetate. The safe daily limit for preformed vitamin A during pregnancy is 10,000 IU. Most prenatal vitamins contain around 2,500 IU, which is acceptable if you’re not eating liver or taking extra supplements.
Is isotretinoin (Accutane) ever safe during pregnancy?
No. Isotretinoin is classified as Pregnancy Category X by the FDA, meaning it’s proven to cause severe birth defects and should never be used during pregnancy. Even a single dose during the first trimester can lead to major malformations. Women on isotretinoin must use two forms of birth control and have monthly pregnancy tests.
How long after stopping isotretinoin can I get pregnant?
You should wait at least one month after your last dose. However, because isotretinoin can linger in fat tissue, some doctors recommend waiting three months to be extra safe. The iPLEDGE program requires one month, but individual risk tolerance may vary. Always consult your doctor before trying to conceive.
Are topical retinoids like tretinoin cream dangerous in pregnancy?
The risk is extremely low. Studies show that topical tretinoin results in blood levels below detectable limits (<0.5 ng/mL). While manufacturers advise caution, there are no confirmed cases of birth defects from topical use alone. Still, many doctors recommend switching to safer alternatives like azelaic acid or bakuchiol during pregnancy to eliminate any theoretical risk.
What foods are high in preformed vitamin A and should be avoided?
Beef liver (3 oz = 27,000 IU), cod liver oil (1 tsp = 13,500 IU), chicken liver, and fortified dairy products. Even one serving of liver exceeds the daily limit for pregnant women. Avoid these entirely during pregnancy. Fish like swordfish and king mackerel also contain high levels. Beta-carotene-rich foods like carrots, sweet potatoes, and spinach are safe and encouraged.
Why is beta-carotene safe but retinol isn’t?
Your body converts beta-carotene into vitamin A only as needed. If you have enough, it stops converting. Retinol, however, is already active. Your body can’t regulate how much it stores-it just absorbs and stores it in the liver. That’s why excess retinol builds up over time and can reach toxic levels, especially during pregnancy.
What should I do if I took vitamin A supplements before knowing I was pregnant?
Don’t panic. If you took a standard prenatal vitamin with 2,500-5,000 IU of retinol and didn’t eat liver or take extra supplements, your risk is very low. But if you took high-dose supplements (10,000 IU or more daily) or consumed liver regularly, talk to your OB-GYN. They may recommend a detailed ultrasound to check for structural abnormalities, especially between weeks 18-22.
Are there any safe vitamin A alternatives for skin during pregnancy?
Yes. Bakuchiol is a plant-based ingredient that mimics retinol’s effects without the risks. Azelaic acid helps with acne and redness. Niacinamide reduces inflammation and improves skin barrier function. These are all considered safe and effective during pregnancy. Look for products labeled “pregnancy-safe” or ask your dermatologist for recommendations.




9 Comments