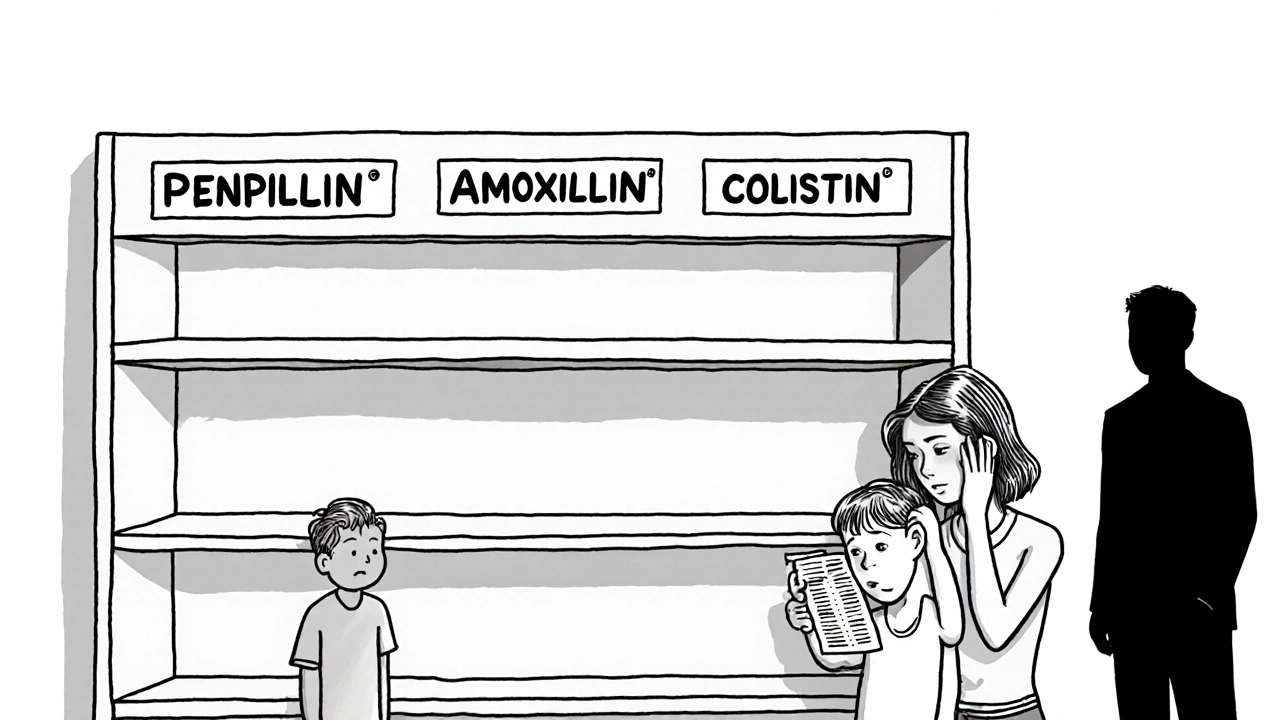
Antibiotic shortages are leaving infections untreated, driving resistance, and costing lives. From penicillin to amoxicillin, critical drugs are vanishing - and the consequences are deadly. Here’s how global supply chains, economics, and resistance are colliding.
Antibiotic Access: How to Get the Right Medication When You Need It
When you’re sick and your doctor says you need an antibiotic, a medicine designed to kill or stop the growth of bacteria that cause infections. Also known as antibacterial agents, they’re one of the most important tools in modern medicine — but getting them isn’t always easy. Many people assume antibiotics are just a quick trip to the pharmacy, but the reality is more complicated. Access to these drugs now depends on where you live, whether you have insurance, how strict local regulations are, and even how often doctors are willing to prescribe them.
Overuse and misuse of antibiotic resistance, the ability of bacteria to survive and multiply despite antibiotic treatment have forced health systems to tighten controls. What used to be a simple prescription is now often a conversation — and sometimes a delay. In some places, you can’t even walk into a pharmacy and buy antibiotics without a valid script. That’s good for public health, but it leaves people in urgent need feeling stuck. Meanwhile, others in underserved areas struggle to find any pharmacy that stocks affordable versions, especially generics like amoxicillin or doxycycline. The gap between needing an antibiotic and actually getting one is wider than most realize.
Low-cost antibiotic access, the ability to obtain necessary antibiotics at an affordable price without unnecessary delays or barriers isn’t just about price — it’s about timing, location, and awareness. Community clinics, mail-order pharmacies, and telehealth services are stepping in to fill gaps, especially for people without insurance. Some apps now let you get a prescription after a quick video visit, and others offer discount programs for common antibiotics. But knowing where to look, what questions to ask, and how to spot a scam is just as important as knowing which drug you need.
What you won’t find in most doctor’s offices is advice on how to avoid needing antibiotics in the first place. That’s why many of the posts here focus on alternatives, prevention, and managing symptoms without rushing to antibiotics. You’ll read about how diet, hydration, and rest can sometimes do the job — and why pushing for a prescription when it’s not needed can hurt you later. There are also real stories from people who waited too long for treatment, or who got the wrong antibiotic because they couldn’t afford the right one.
And it’s not just about getting the drug — it’s about getting the right one. Not every infection needs an antibiotic. Viral colds, flu, and most sore throats won’t respond to them. Yet people still ask for them. Doctors still sometimes give them. That’s how resistance grows. The posts here cut through the noise: they show you how to tell when antibiotics are truly needed, how to talk to your provider about alternatives, and where to find safe, legal, and affordable options without falling for online scams or counterfeit pills.
Whether you’re dealing with a stubborn sinus infection, a UTI that won’t go away, or just worried about what happens if you can’t get your next dose, this collection gives you real, practical answers. You’ll find guides on free clinics, how to compare generic brands, what to do if your pharmacy runs out, and even how to spot misleading ads for "miracle" antibiotics online. No fluff. No hype. Just what works — and what doesn’t — when your health is on the line.