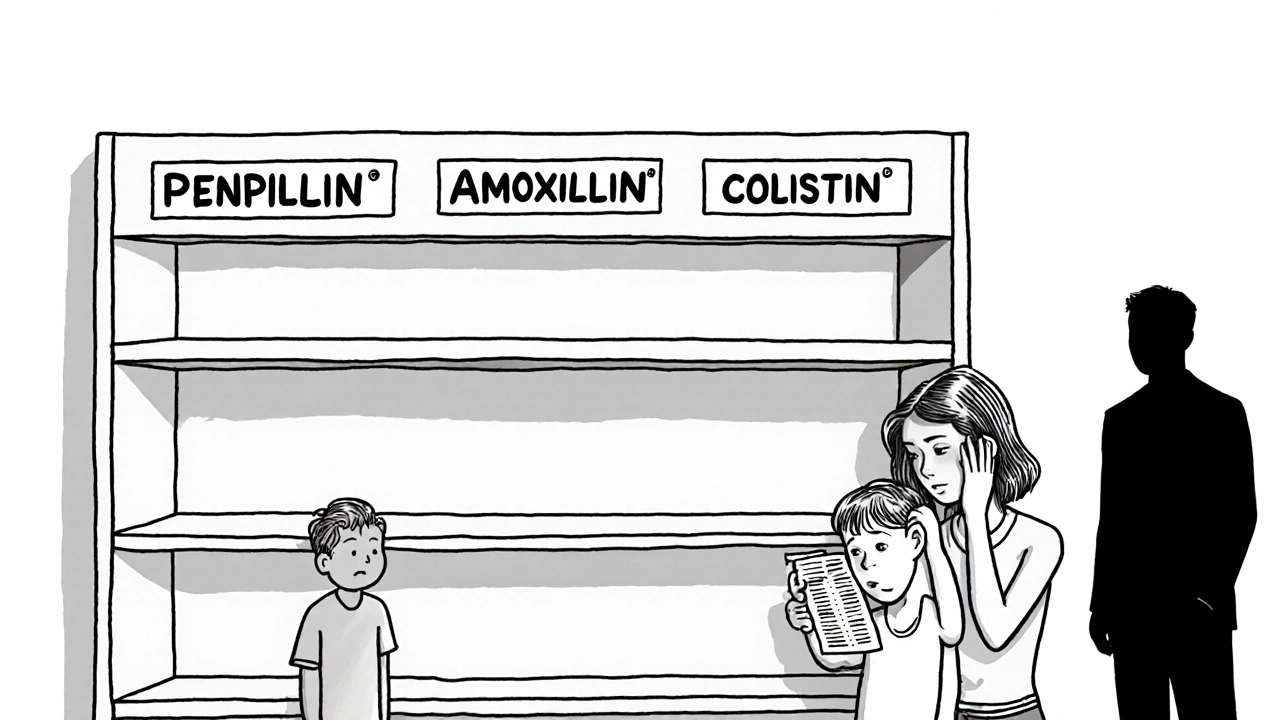
Antibiotic shortages are leaving infections untreated, driving resistance, and costing lives. From penicillin to amoxicillin, critical drugs are vanishing - and the consequences are deadly. Here’s how global supply chains, economics, and resistance are colliding.
Antibiotic Resistance: What It Is, Why It Matters, and How It’s Changing Treatment
When antibiotic resistance, the ability of bacteria to survive drugs designed to kill them. Also known as drug-resistant infections, it means antibiotics that once worked like magic now fail—leaving simple infections dangerous and even deadly. This isn’t science fiction. It’s happening right now, in hospitals, homes, and farms around the world. Every time you take an antibiotic when you don’t need it—or don’t finish the full course—you’re helping bacteria learn how to fight back.
Antibiotic resistance doesn’t happen because your body changes—it’s the bacteria, microscopic organisms that can adapt and multiply rapidly that evolve. Some survive the drug, pass on their resistance genes, and soon, entire strains become untouchable. These are the superbugs, bacteria that resist multiple antibiotics, including last-resort drugs. MRSA, VRE, and drug-resistant tuberculosis aren’t rare outliers—they’re growing fast. The World Health Organization calls antibiotic resistance one of the biggest threats to global health.
It’s not just about hospitals. Antibiotics are overused in farming, where they’re fed to animals to make them grow faster or prevent disease in crowded conditions. That resistance doesn’t stay on the farm—it gets into water, soil, and eventually, your food. Even more troubling? Many people still believe antibiotics work for colds or flu. They don’t. Those are viruses. Taking antibiotics for a virus doesn’t help you—it just gives bacteria more chances to build defenses.
What does this mean for you? If you get a serious infection in 10 years, the drugs your doctor reaches for might not work. Simple surgeries, chemotherapy, even a cut that gets infected could become life-threatening again. That’s why the fight against antibiotic resistance isn’t just for doctors or scientists—it’s for everyone who’s ever taken a pill.
Some of the posts below show how medications like doxepin or lisinopril-HCTZ affect your body, but none of them work if the tools we rely on—antibiotics—stop working. You’ll find real stories here about how people manage chronic conditions, avoid side effects, and navigate complex drug systems. But behind every treatment plan, there’s one silent question: will the next antibiotic still work?
What follows isn’t just a list of articles—it’s a snapshot of how modern medicine is adapting, struggling, and sometimes failing to keep up. You’ll learn about safe prescribing, how to spot when antibiotics are truly needed, and why your choices matter more than you think. This isn’t about fear. It’s about awareness. And awareness is the first dose that actually works.