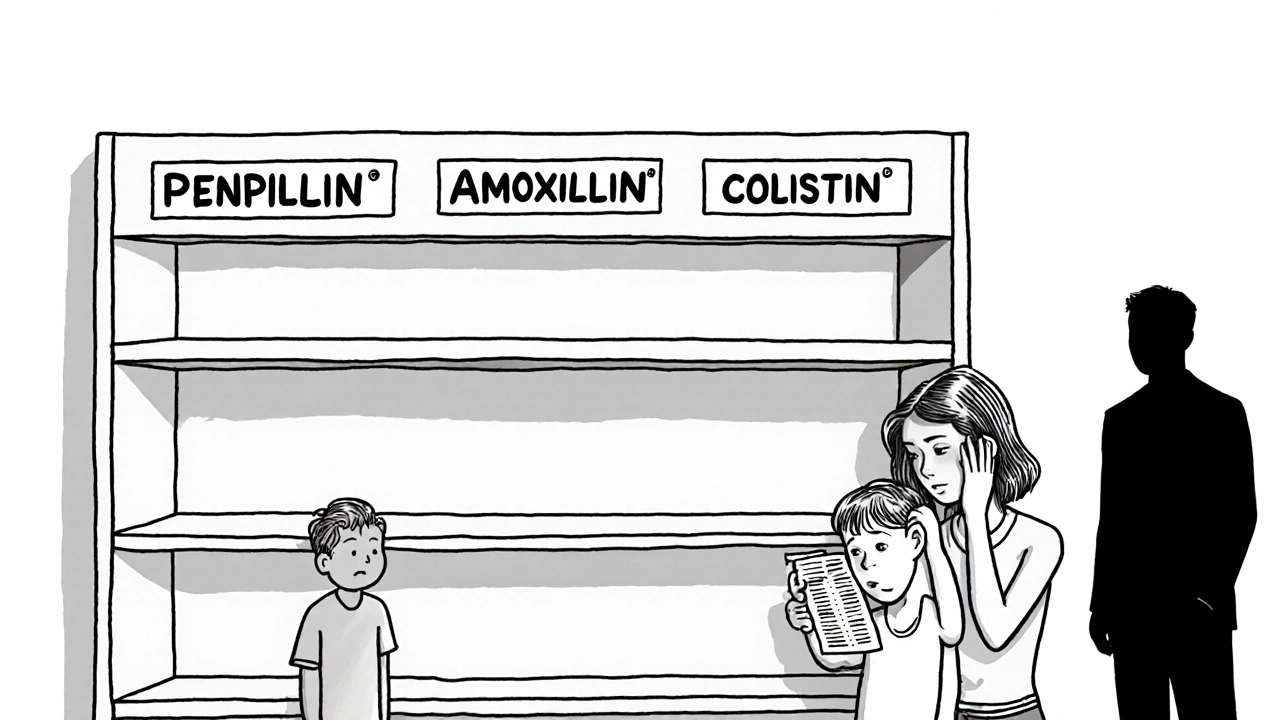
Antibiotic shortages are leaving infections untreated, driving resistance, and costing lives. From penicillin to amoxicillin, critical drugs are vanishing - and the consequences are deadly. Here’s how global supply chains, economics, and resistance are colliding.
Antibiotic Shortages: What’s Causing Them and How to Cope
When your doctor prescribes an antibiotic, a medicine used to treat bacterial infections. Also known as antibacterial agents, these drugs save lives by killing or stopping the growth of harmful bacteria. But lately, getting that prescription filled has become harder. Antibiotic shortages, a growing problem where essential drugs aren’t available in pharmacies are no longer rare. They’re affecting everything from simple urinary tract infections to serious pneumonia cases. And it’s not just about running out of stock—it’s about broken supply chains, manufacturing delays, and rising costs.
Why does this keep happening? One big reason is antibiotic resistance, when bacteria evolve to survive common drugs. As older antibiotics lose effectiveness, manufacturers shift focus to newer, more profitable ones. That leaves older, cheaper antibiotics—like amoxicillin or doxycycline—underproduced. Even small disruptions, like a factory shutdown or raw material shortage, can cause ripple effects. The U.S. Food and Drug Administration tracks these gaps, and in 2023 alone, over 200 antibiotics were listed as in short supply. Many of these are generics, which pharmacies rely on because they’re affordable. But when production stops, there’s often no backup.
It’s not just patients who feel the pinch. Doctors are forced to switch treatments on the fly, sometimes using less effective or more expensive alternatives. Seniors, kids, and people with chronic illnesses are hit hardest. If you’re on a long-term antibiotic regimen, or need one for an infection, you might find your usual drug gone. That’s when knowing your options matters. Some shortages are temporary, but others last months. In the meantime, community clinics and discount pharmacy programs can help you find alternatives. You might also get lucky with a different brand or formulation—like switching from a pill to a liquid if you’re treating a child.
What you can do right now? Don’t panic, but don’t wait either. If your pharmacy says your antibiotic is out of stock, ask for a list of nearby locations that might have it. Call your doctor immediately—many can prescribe a similar drug from another class. Also, check if your insurance covers a substitute. And remember: never take leftover antibiotics or share prescriptions. That only makes resistance worse. The system is strained, but there are still ways to get what you need. Below, you’ll find real stories and practical advice from people who’ve navigated these gaps, plus guides on how to find low-cost options, understand FDA alerts, and work with your healthcare team when drugs aren’t available.