Asthma Inhaler Substitution: Safe Switches, Alternatives, and What to Watch For
When your asthma inhaler substitution, the process of replacing one inhaler with another due to cost, availability, or side effects. Also known as asthma medication switch, it’s something many people with asthma face at least once—whether because their insurance changed, the brand was pulled from shelves, or their doctor wants to try something cheaper or gentler. It’s not just swapping one device for another. Getting it wrong can mean worse symptoms, more ER visits, or even a life-threatening flare-up.
Most asthma inhalers fall into two main types: bronchodilators, quick-relief drugs that open airways during an attack like albuterol, and corticosteroid inhalers, daily preventers that reduce swelling and mucus in the lungs like fluticasone or budesonide. You can’t swap these types for each other. A rescue inhaler won’t stop daily inflammation, and a steroid inhaler won’t stop sudden wheezing. Substitution only works within the same category. If you’re on albuterol, you might switch to levalbuterol or a generic version—but never to a steroid. That’s a common mistake people make when they’re confused by packaging or told "it’s the same thing."
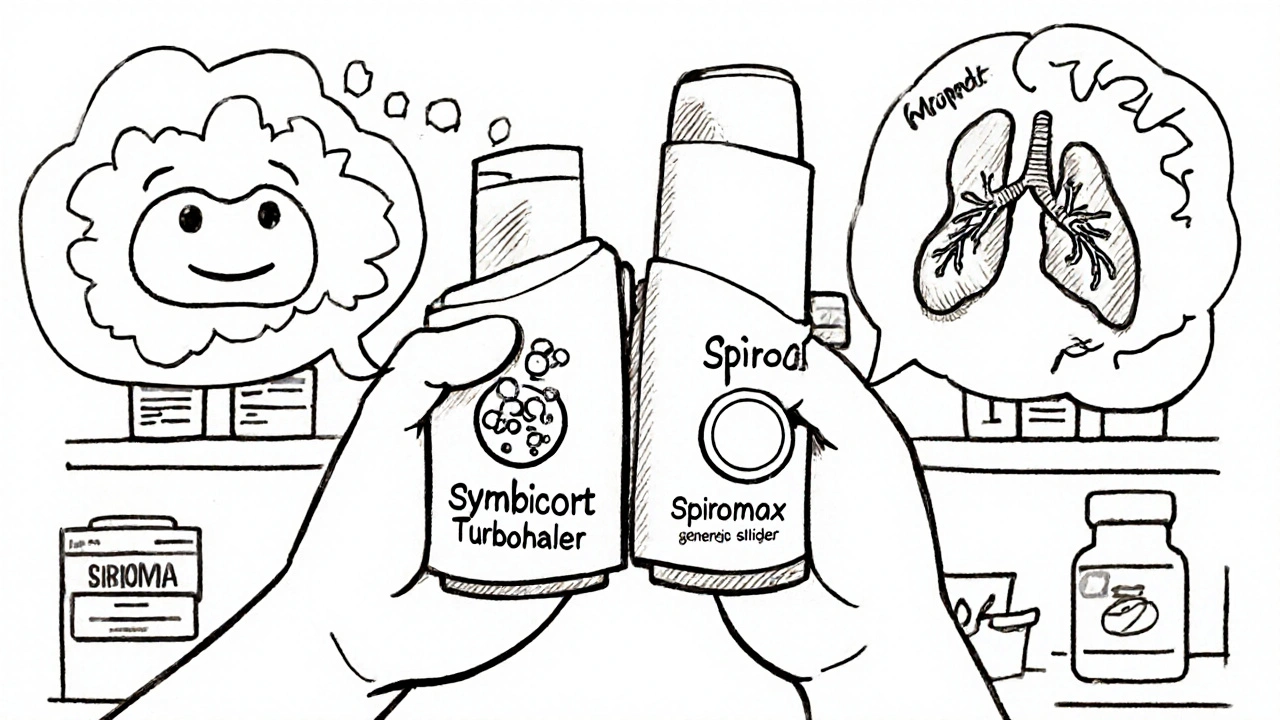
Even within the same type, not all inhalers are equal. Different devices—metered-dose inhalers, dry powder inhalers, nebulizers—require different breathing techniques. If you switch from a press-and-breathe MDI to a dry powder inhaler like Advair Diskus, you need to learn a new method. If you don’t, you’re not getting the full dose. Many patients think they’re taking their medicine correctly until they realize they’ve been inhaling too weakly or too fast. That’s why switching inhalers often comes with a quick training session from a pharmacist or nurse.
Cost is the biggest reason people look for substitutions. Brand-name inhalers like ProAir HFA or Symbicort can cost over $300 without insurance. Generic versions, like albuterol sulfate HFA, can be under $20. But not all generics are created equal. Some have different propellants, particle sizes, or even slightly different dosing. The FDA says they’re equivalent, but real patients report differences in throat irritation, taste, or how long the relief lasts. If your symptoms change after switching, it’s not "all in your head." It’s a real pharmacological difference.
Some substitutions happen because of supply issues. In 2023, shortages of certain albuterol inhalers forced clinics to switch patients to alternative brands overnight. Others switch because of side effects—like a dry mouth from steroids or a racing heart from bronchodilators. You might need to try two or three options before finding one that feels right. Don’t settle for discomfort. Talk to your doctor about alternatives like the newer ProAir Respiclick or the non-fluorocarbon inhalers now available.
What you shouldn’t do is switch on your own. Even if two inhalers look similar, they might have different strengths, dosing schedules, or warnings. One might be approved for kids under 12, another only for adults. One might require a spacer, another doesn’t. Mixing up these details can be dangerous. Always get your substitution approved by your provider and double-check the label when you pick it up.
Below, you’ll find real patient experiences and expert breakdowns on common asthma inhaler swaps, what works, what doesn’t, and how to spot red flags when your medication changes. Whether you’re dealing with a new insurance plan, a drug shortage, or just tired of side effects, these guides help you take control without risking your health.