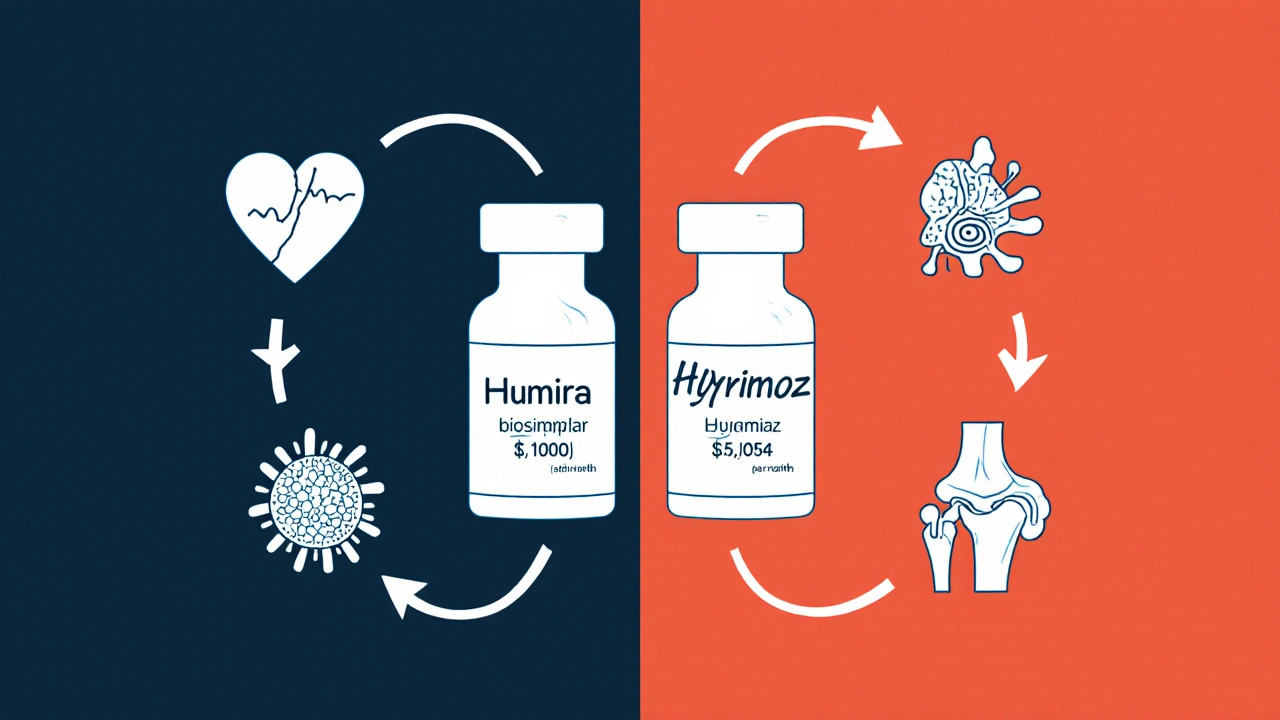
Biosimilars are highly similar, lower-cost versions of complex biologic drugs. They offer proven safety and effectiveness with 15-30% savings, helping patients access treatments for cancer, arthritis, and autoimmune diseases without sacrificing quality.
Biologic Drugs: What They Are, How They Work, and What You Need to Know
When you hear biologic drugs, medications made from living organisms like cells or proteins, not synthesized in a lab like traditional pills. Also known as biologics, they’re engineered to target specific parts of your immune system or disease pathways. Unlike regular pills that circulate broadly, biologics act like precision tools—homing in on the exact cells or proteins causing harm. That’s why they’re used for serious conditions like rheumatoid arthritis, psoriasis, Crohn’s disease, and certain cancers. But because they’re so powerful, they also come with unique risks and requirements.
These drugs are often given by injection or IV because your stomach breaks them down if you swallow them. They’re not interchangeable with generics—there’s no such thing as a "generic biologic" yet. Instead, you might hear about "biosimilars," which are highly similar but not identical copies. The autoimmune diseases, conditions where your immune system attacks your own body. Also known as immune disorders, they are the most common targets for biologics. Drugs like adalimumab or etanercept block TNF-alpha, a protein that fuels inflammation. For cancer, drugs like rituximab or trastuzumab tag cancer cells so your immune system can find and destroy them. But because they suppress parts of your immune system, you’re more vulnerable to infections. That’s why doctors check for TB or hepatitis before starting treatment.
Another big concern is drug interactions, how biologics react with other medications, supplements, or even vaccines. Also known as medication conflicts, they can be unpredictable. For example, mixing biologics with other immune-suppressing drugs can raise infection risk. Even over-the-counter herbs or supplements like green tea extract or turmeric might interfere. And you can’t get live vaccines—like the shingles or MMR shot—while on these drugs. That’s why tracking every pill, patch, or shot you take is critical.
Biologic drugs changed how we treat chronic illness. They’ve given people back mobility, reduced flare-ups, and even saved lives. But they’re not magic. They need careful monitoring, strict schedules, and honest conversations with your doctor. The posts below cover real-world issues: how biologics interact with other treatments, what side effects to watch for, why some people stop them, and how to manage costs and access. Whether you’re on one now or just starting to learn, this collection gives you the facts you need to stay safe and informed.