Biologic drugs have changed how we treat serious conditions like rheumatoid arthritis, Crohn’s disease, and certain cancers. But they come with a steep price tag - sometimes over $7,000 a month. That’s where biosimilars come in. They’re not generics. They’re not copies. They’re highly similar versions of these complex medicines, approved by the FDA to work the same way, with no meaningful difference in safety or effectiveness. And they’re starting to make these life-changing treatments more affordable.
What Exactly Are Biosimilars?
Biosimilars are made from living cells - yeast, bacteria, or animal cells - not chemicals. That’s why they’re so different from regular generic pills. A generic version of aspirin is chemically identical to the brand name. But a biosimilar can’t be identical to its reference biologic because living systems are messy. Even tiny changes in temperature, pH, or fermentation time during manufacturing can affect the final product.
The FDA doesn’t require biosimilars to be identical. They just need to be highly similar - with no clinically meaningful differences in how they work, how safe they are, or how effective they are. To prove this, manufacturers run hundreds of tests: comparing protein structures, checking how the drug behaves in the body, studying immune responses, and running clinical trials on thousands of patients.
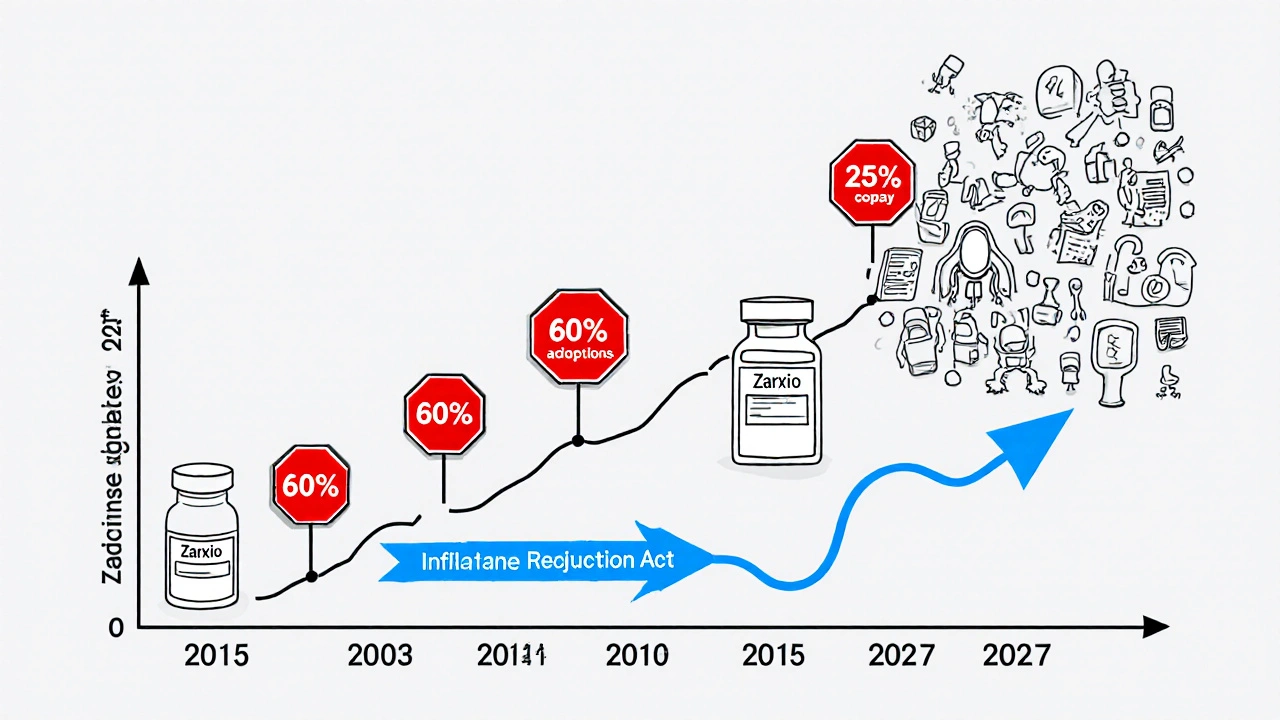
The first biosimilar approved in the U.S. was Zarxio in 2015, a version of filgrastim used to boost white blood cells after chemotherapy. Since then, the FDA has approved 45 biosimilars as of October 2023. These cover treatments for cancer, autoimmune diseases, and diabetes.
How Do Biosimilars Save Money?
Biologics are expensive because they’re hard to make. Developing one can cost over $2 billion and take more than a decade. Biosimilars don’t need to repeat all that expensive research. They build on the existing data from the original drug, which cuts development time and cost.
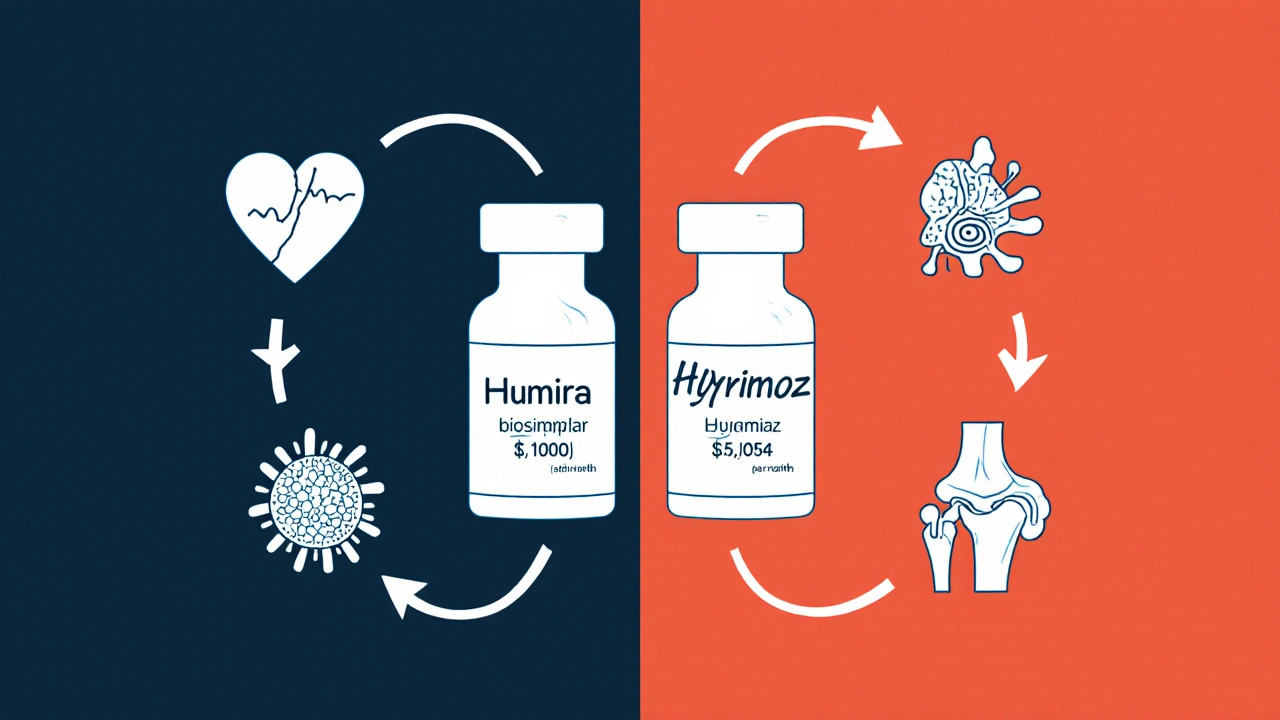
But don’t expect 80% price drops like with generics. Biosimilars typically launch at 15% to 30% lower than the reference drug. For example, when Humira biosimilars hit the U.S. market in 2023, their list price was around $5,054 per month - 28% less than Humira’s $7,000. That’s still a lot, but it adds up fast when you’re talking about millions of patients.
The real savings come from competition. Once more biosimilars enter the market, prices drop further. In Europe, where biosimilars have been around longer, the filgrastim market is 84% biosimilar - and prices fell by over 70%. In the U.S., it’s slower. For infliximab (Remicade), biosimilars captured 72% of new prescriptions within 18 months. But for etanercept (Enbrel), aggressive patent lawsuits slowed adoption. Market access barriers like this keep U.S. savings lower than in Europe.
The Congressional Budget Office estimates biosimilars could save U.S. healthcare $150 billion annually by 2030 - if we remove those barriers.
Are Biosimilars Safe?
This is the biggest question patients ask. The answer, backed by science: yes.
The FDA requires biosimilars to meet the same high standards as the original. Studies show no increased risk of side effects. The NOR-SWITCH trial, published in The Lancet in 2016, followed over 500 patients who switched from a reference biologic to a biosimilar. No increase in immune reactions, flare-ups, or hospitalizations.
Dr. Gary Lyman, a cancer researcher at Fred Hutchinson Cancer Center, reviewed data from dozens of trials and concluded: “Biosimilars have demonstrated equivalent efficacy and safety profiles compared to their reference products across multiple clinical trials involving thousands of patients.”
The European Medicines Agency has tracked biosimilars for over 16 years. No unexpected safety issues have emerged.
But here’s the catch: switching matters. If you’ve been stable on a biologic for years, switching to a biosimilar should be done with your doctor’s guidance. While single switches are safe, multiple switches between different biosimilars or the original drug need more monitoring. As Dr. Almut Winterstein from the University of Florida notes, “While single-switch studies show comparable outcomes, multiple switches require additional monitoring.”
Interchangeable vs. Biosimilar: What’s the Difference?
The FDA has two categories: biosimilar and interchangeable biosimilar.
All interchangeable biosimilars are biosimilars, but not all biosimilars are interchangeable. To be labeled interchangeable, a product must prove it can be switched back and forth with the reference drug without increasing risk. It must also be able to be substituted at the pharmacy without the prescriber’s involvement - just like a generic.
As of November 2023, only six biosimilars have this designation. The first interchangeable Humira biosimilar, Hyrimoz, was approved in July 2023. That’s a big deal. It means pharmacists can swap it for Humira without calling the doctor - if state laws allow it.
Forty-eight states have laws governing biosimilar substitution. Most require the pharmacist to notify the prescriber and patient. Some require patient consent. The rules vary, so it’s not automatic everywhere.
What Do Patients Actually Experience?
Real-world data from patient surveys tells a clear story.
The Arthritis Foundation surveyed 1,200 people using biosimilars. 87% said they saw no difference in effectiveness compared to the original biologic. 72% reported lower out-of-pocket costs. That’s huge for people paying hundreds or thousands per month.
But 28% had initial fears. Common concerns: “Will this work as well?” “Will I have side effects?” “Is this a cheaper version?”
Those fears dropped after talking to their doctor. One Reddit user in r/rheumatology wrote: “I was terrified to switch from Remicade. My rheumatologist spent 15 minutes showing me the data. Now I’m on Renflexis - same results, half the cost.”
On Drugs.com, Renflexis has a 4.2/5 rating from over 140 reviews. The complaints? Insurance denials. Prior authorizations. Delays in getting coverage. Not lack of effectiveness.
Why Aren’t More People Using Them?
It’s not because they don’t work. It’s because the system is complicated.
Doctors need training. A 2022 ASCO survey found 78% of oncologists needed 1-2 hours of education before feeling comfortable prescribing biosimilars. The biggest hurdle? “Navigating payer-specific coverage requirements.”
Insurance companies often have rules that favor the brand-name drug. They might require you to try the biosimilar first (step therapy). Or they might not cover it unless the doctor checks a box or fills out extra paperwork.
Pharmaceutical companies also use tactics to delay biosimilar entry - patent thickets, lawsuits, and “product hopping” - where they tweak the original drug slightly and launch a new version just before biosimilars hit the market.
And then there’s the marketing. Biologic manufacturers spend billions on ads and patient support programs. Biosimilar makers have far less budget. Many patients simply don’t know biosimilars exist.
What’s Next?
The next wave is coming. High-revenue biologics like Stelara (ustekinumab), Enbrel, and Kyntheum are about to face biosimilar competition. Seven biosimilar applications for Stelara are pending FDA review as of September 2023.
The Inflation Reduction Act of 2022 is helping. Starting in 2024, Medicare Part D patients will pay only 25% out-of-pocket for biosimilars - down from 50% or more. That’s a major incentive for patients and insurers.
By 2027, experts predict biosimilar adoption could rise from 25-30% to 50-60% for most products. That means more people getting the treatment they need without financial ruin.
The future might even include “biobetters” - next-gen biologics with improved properties. But those won’t replace biosimilars. They’ll compete with both the original and the biosimilar.
Where to Find Reliable Information
Don’t trust manufacturer ads alone. Use trusted sources:
- FDA Purple Book - The official list of all approved biosimilars and their reference products.
- Biosimilars Council - Free toolkits by disease (arthritis, cancer, etc.) with patient and provider guides.
- World Health Organization (WHO) - Global standards and guidelines.
- Arthritis Foundation and American Cancer Society - Patient-friendly summaries.
If your doctor hasn’t mentioned biosimilars, ask. Say: “Is there a biosimilar option for my medication? What’s the cost difference? Is it covered?”
Are biosimilars the same as generics?
No. Generics are chemically identical copies of small-molecule drugs like aspirin or metformin. Biosimilars are highly similar versions of complex biologic drugs made from living cells. They can’t be exact copies because of their complexity, but they work the same way and are equally safe and effective.
How much cheaper are biosimilars than brand-name biologics?
Biosimilars typically launch at 15% to 30% lower than the original biologic. For example, Humira biosimilars started at about $5,054 per month compared to Humira’s $7,000. Prices drop further as more biosimilars enter the market. Savings vary by drug, insurer, and state laws.
Can I switch from a biologic to a biosimilar safely?
Yes, for most people. Multiple studies, including the large NOR-SWITCH trial, show no increased risk of side effects or loss of effectiveness when switching from a reference biologic to a biosimilar. However, switching multiple times - back and forth between different products - requires careful monitoring by your doctor.
Why isn’t my insurance covering my biosimilar?
Insurance companies sometimes favor the brand-name drug through prior authorization, step therapy, or formulary restrictions. Even if a biosimilar is cheaper, your plan may require you to try the original first. Talk to your doctor about appealing the decision or asking for a formulary exception.
Are biosimilars approved outside the U.S.?
Yes. The European Medicines Agency (EMA) approved the first biosimilar in 2006. Many countries, including Canada, Australia, and Japan, have robust biosimilar approval systems. Europe has higher adoption rates than the U.S. due to different pricing and reimbursement rules.
Will biosimilars work for my specific condition?
Biosimilars are approved for the same conditions as their reference biologics - including rheumatoid arthritis, Crohn’s disease, psoriasis, and certain cancers. But not every biologic has a biosimilar yet. Check the FDA Purple Book or ask your doctor if a biosimilar exists for your medication.
Do biosimilars have more side effects?
No. The FDA requires extensive testing to ensure biosimilars have no increased risk of side effects. Studies involving thousands of patients show their safety profiles match the original biologic. Concerns about immune reactions have been largely disproven by real-world data.
What You Can Do Now
If you’re on a biologic, ask your doctor: “Is there a biosimilar available for my drug?” If you’re about to start one, ask: “Are there lower-cost biosimilar options?”
Check your insurance plan’s formulary. Look up your drug in the FDA Purple Book. Talk to your pharmacist. These steps can save you thousands a year - without compromising your health.








8 Comments