When you’re facing cancer surgery, one of the most important decisions isn’t about the scalpel-it’s about when to give treatment. Should you start chemotherapy or immunotherapy before the operation, or wait until after? This isn’t just a technical question. It’s about survival, side effects, and knowing if the treatment is even working. For many patients with lung or breast cancer, the answer today isn’t one-size-fits-all. It’s shaped by tumor type, biomarkers, and the latest clinical evidence.
What Neoadjuvant Therapy Actually Does
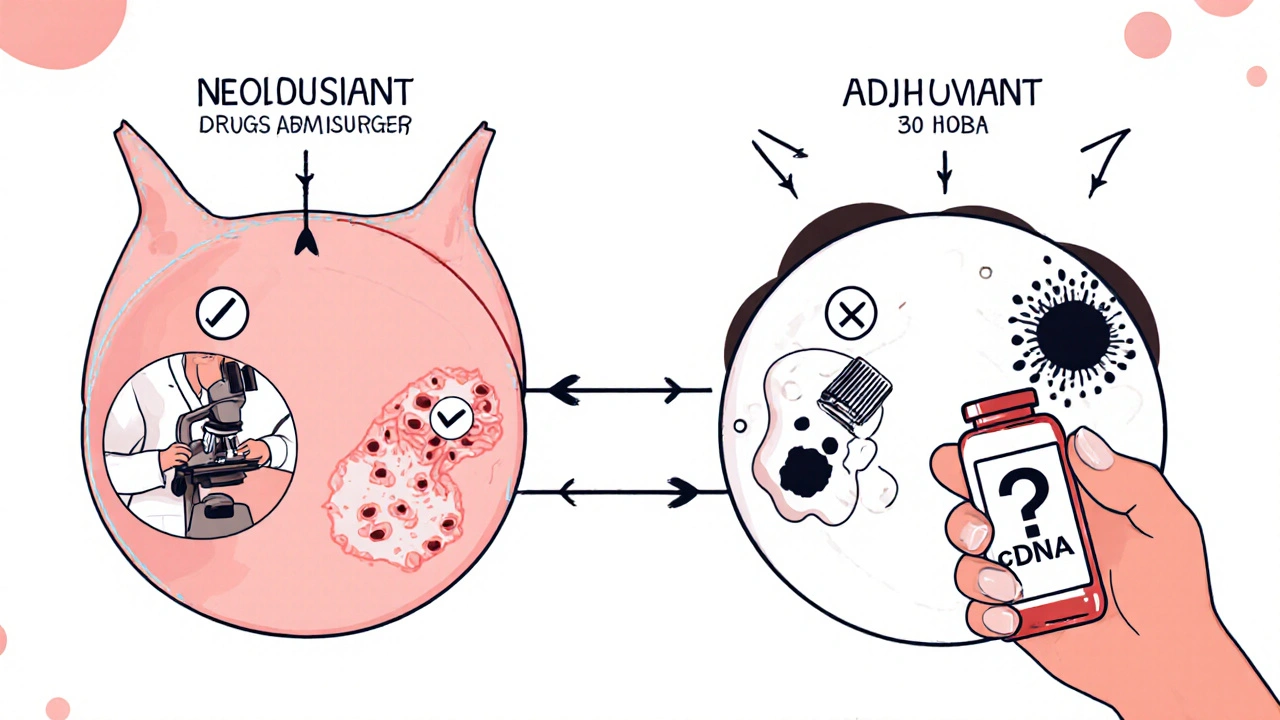
Neoadjuvant therapy means treatment given before surgery. It’s not just a way to shrink a tumor so it’s easier to remove. It’s a real-time test. You give the drugs, then watch what happens. If the tumor shrinks dramatically-or even disappears-you know the cancer is sensitive to that treatment. That’s valuable information you can’t get any other way.
In non-small cell lung cancer (NSCLC), the CheckMate 816 trial changed everything. Patients who got nivolumab (an immunotherapy) plus chemotherapy before surgery had a 24% rate of pathologic complete response (pCR)-meaning no living cancer cells were found in the removed tissue. That’s compared to just 2.2% with chemo alone. And those who achieved pCR had a much better chance of staying cancer-free. The same pattern holds for triple-negative breast cancer. About 30-40% of patients reach pCR with neoadjuvant chemo, and those patients live longer.
It’s not just about killing cancer cells early. Neoadjuvant therapy also hits micrometastases-tiny clusters of cancer that have already spread but are too small to see on scans. By attacking them before surgery, you reduce the chance they’ll grow back later. And because you’re treating the tumor while it’s still in place, the immune system gets a better chance to respond.
Why Adjuvant Therapy Still Matters
Adjuvant therapy is given after surgery. Its goal is simple: wipe out any cancer cells left behind. Even if the surgeon removed everything visible, there could be a few rogue cells hiding in the body. That’s where chemo, hormone therapy, or immunotherapy comes in.
For decades, adjuvant therapy was the standard. It worked. But it had a big flaw-you didn’t know if the drugs were working until months later, when a scan showed a recurrence. With neoadjuvant therapy, you find out quickly. If the tumor doesn’t respond, you can switch treatments before surgery. With adjuvant therapy, you’re stuck with a plan that might not have been right for your cancer.
That’s why the tide is turning. But adjuvant therapy isn’t going away. For some patients, especially those with poor response to neoadjuvant treatment, it’s still essential. Dr. David Harpole from Duke University points out that even after neoadjuvant therapy, micrometastases can linger. That’s why some doctors still recommend continuing immunotherapy after surgery.
The Big Shift: Neoadjuvant-Only Is Gaining Ground
In early 2024, a major analysis of four trials-KEYNOTE-671, Neotorch, AEGEAN, and NADIM II-looked at over 3,200 patients with resectable NSCLC. The results surprised many. Patients who got immunotherapy only before surgery did just as well as those who got it before and after. Survival rates were nearly identical. But the group that got extra treatment after surgery had way more serious side effects: nearly 30% had grade 3 or higher toxicities, compared to under 18% in the neoadjuvant-only group.
This isn’t just a statistical finding. Real patients are noticing the difference. One NSCLC patient from the Cancer Survivors Network said, “My oncologist recommended neoadjuvant nivolumab plus chemo because it gave us a chance to see if the treatment worked before surgery-turns out I had a major pathologic response (>90% tumor kill), which was reassuring.”
Dr. Mark Awad from Dana-Farber Cancer Institute put it bluntly: “The neoadjuvant-only approach may represent the optimal sequencing strategy for early-stage NSCLC, sparing patients unnecessary toxicity without compromising efficacy.”
That’s why guidelines are changing. The FDA approved neoadjuvant nivolumab plus chemo for NSCLC in March 2022. The European Medicines Agency followed later that year. And by 2023, 78% of community oncologists in the U.S. were offering neoadjuvant immunotherapy for stage II-III NSCLC-up from just 42% in 2021.
Where Breast Cancer Fits In
Breast cancer has been using neoadjuvant therapy longer than lung cancer. It’s standard for HER2-positive and triple-negative subtypes, especially if the tumor is large or has spread to lymph nodes. The goal? Make surgery less disfiguring and find out if the tumor responds.
Studies comparing neoadjuvant and adjuvant therapy in early-stage triple-negative breast cancer found no big difference in overall survival. But here’s the catch: patients who achieved pCR after neoadjuvant therapy lived significantly longer than those who didn’t. That’s why neoadjuvant therapy isn’t just about shrinking tumors-it’s about risk stratification. If your cancer doesn’t respond, you’re flagged as high-risk. That means you get more aggressive treatment afterward.
For hormone receptor-positive breast cancer, neoadjuvant therapy is less common, but it’s growing. If a tumor is too big to remove cleanly, doctors use chemo or hormone blockers first to shrink it. That way, more women can have breast-conserving surgery instead of a mastectomy.
Who Gets Which Treatment?
It’s not random. Guidelines from the National Comprehensive Cancer Network (NCCN) say neoadjuvant chemoimmunotherapy should be offered to patients with stage IB (tumor ≥4 cm) to IIIA NSCLC. For breast cancer, the Society of Surgical Oncology recommends it for HER2-positive, triple-negative, or large hormone-positive tumors.
But access isn’t equal. A 2023 study found only 58% of community hospitals have formal neoadjuvant pathways. Academic centers? 92%. That gap means patients in rural or under-resourced areas may still be getting outdated care.
Also, timing matters. After neoadjuvant therapy, surgery should happen 3 to 6 weeks later. Too soon, and tissues are still inflamed. Too late, and the cancer might start growing again. And you need experts to interpret scans and pathology reports. Radiologists use RECIST criteria. Pathologists use Miller-Payne grading for breast cancer or the American College of Pathologists system for lung tissue. If those aren’t done right, you’re flying blind.
The Future: ctDNA and Personalized Sequencing
The next big leap? Blood tests. Circulating tumor DNA (ctDNA) can detect cancer cells in the bloodstream-even when scans are clean. Trials like NeoADAURA (testing osimertinib in EGFR-mutant NSCLC) and KEYNOTE-867 are now using ctDNA to decide who needs more treatment after surgery.
Imagine this: You get neoadjuvant therapy. After surgery, a blood test shows no traces of ctDNA. You’re low risk. You stop treatment. But if ctDNA is still there? You get a second round of chemo or immunotherapy. No guessing. No unnecessary side effects.
Dr. Roy Herbst from Yale predicts that within five years, biomarker-driven neoadjuvant therapy will be standard for 70% of early-stage NSCLC cases. Adjuvant therapy will be reserved only for those who show signs of lingering disease.
By 2030, experts estimate optimized sequencing could boost 5-year survival for early-stage lung cancer from 60-68% to 75-80%. That’s 15,000 to 20,000 more lives saved every year in the U.S. alone.
What You Should Ask Your Doctor
If you’re facing surgery for lung or breast cancer, here’s what to ask:
- Is neoadjuvant therapy an option for my cancer type and stage?
- What’s my tumor’s biomarker status? (PD-L1, HER2, EGFR, etc.)
- Will we test for pathologic response after treatment?
- What are the risks of delaying surgery?
- Will you use ctDNA testing to guide next steps?
- Do you have a multidisciplinary team that handles neoadjuvant cases regularly?
Don’t assume the first plan offered is the best. Ask for the evidence. Ask about clinical trials. Ask what happens if the tumor doesn’t shrink. Your treatment plan should be a conversation-not a script.
Final Thoughts
Neoadjuvant and adjuvant therapy aren’t enemies. They’re tools. The best approach depends on your cancer’s biology, your body’s response, and the expertise of your care team. The days of giving chemo after surgery by default are ending. The future is smarter: treat early, measure response, and tailor what comes next. That’s how you turn cancer from a death sentence into a manageable condition.







8 Comments