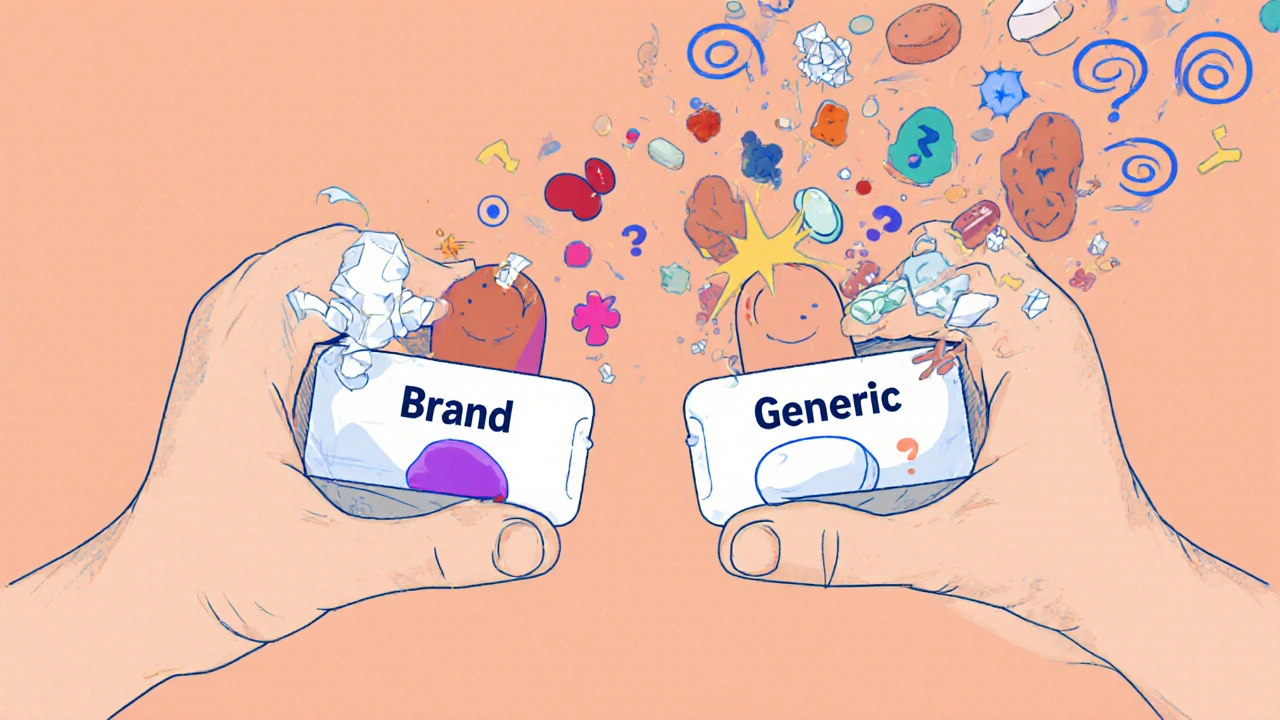
Most people assume that if a generic drug has the same active ingredient as the brand-name version, it will work exactly the same. For the vast majority, that’s true. But for some, switching from a brand to a generic isn’t just a cost-saving move-it can trigger nausea, dizziness, worsening symptoms, or even allergic reactions. And the culprit isn’t the medicine you’re taking. It’s what’s around the medicine.
What Are Excipients, and Why Do They Matter?
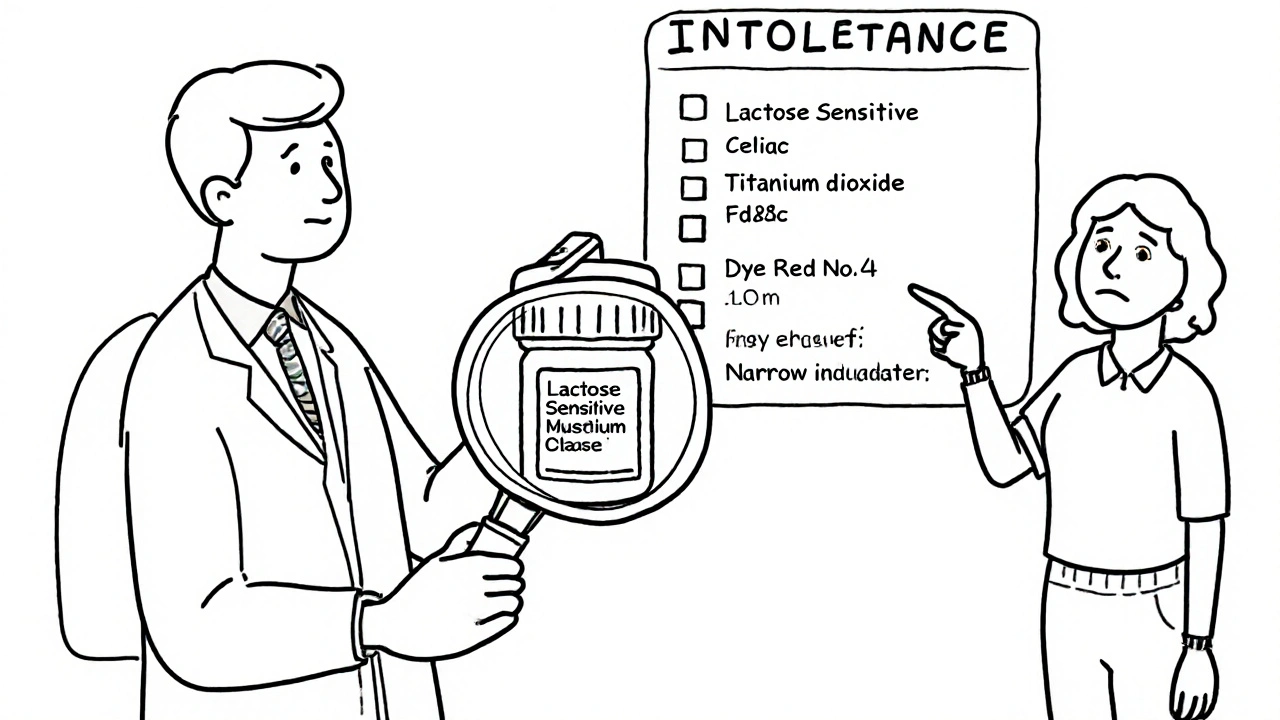
Excipients are the inactive ingredients in pills, capsules, and liquids. They don’t treat your condition. But they do everything else: hold the pill together, make it easier to swallow, help it dissolve at the right speed, give it color, or even preserve it. Common excipients include lactose, corn starch, titanium dioxide, croscarmellose sodium, and artificial dyes like FD&C Red No. 40. The FDA requires generic drugs to match brand-name drugs in active ingredient, strength, dosage form, and how fast the drug enters your bloodstream. But when it comes to excipients? They can be completely different. One company might use lactose as a filler. Another might use mannitol. One brand might use a slow-dissolving coating. The generic might use a fast-dissolving one. These small changes can have big effects-for certain people.When Generic Switching Goes Wrong
For most medications, switching between brand and generic is safe and effective. But not all drugs are created equal. Some have what’s called a narrow therapeutic index-meaning the difference between a dose that works and a dose that’s toxic is tiny. That’s where excipients can cause real problems. Drugs like levothyroxine (for thyroid), warfarin (a blood thinner), and certain anti-seizure medications fall into this category. If a generic version dissolves faster or slower than the brand, your blood levels can dip too low or spike too high. For someone on levothyroxine, that might mean feeling tired, gaining weight, or even developing heart rhythm issues. For someone on an anti-epileptic, it could mean having a seizure. Real-world reports back this up. A 2023 survey by the Michael J. Fox Foundation found that 18% of Parkinson’s patients experienced worse symptoms after switching from branded Sinemet to a generic version of carbidopa/levodopa. One patient on Reddit described severe nausea and dizziness after switching to a generic-symptoms that vanished when they went back to the brand. Why? A different binder in the tablet changed how quickly the drug was absorbed. Another case: a woman with lactose intolerance switched to a generic thyroid medication. The brand used a lactose-free filler. The generic used lactose. Within days, she had bloating, cramps, and diarrhea. Her thyroid levels didn’t change-but her gut did. And because her body couldn’t absorb the medication properly, her symptoms returned.Who’s Most at Risk?
Not everyone will notice a difference. In fact, 78% of people report no change at all when switching to generics, according to GoodRx’s 2023 survey. But certain groups are more vulnerable:- People with known allergies or intolerances to excipients (lactose, gluten, dyes, sulfites)
- Patients on narrow therapeutic index drugs (thyroid meds, blood thinners, anti-seizure drugs, immunosuppressants)
- Those who’ve had bad reactions to a specific generic before
- People with digestive disorders (Crohn’s, celiac, IBS) where absorption is already impaired
- Older adults taking multiple medications-small changes in absorption can pile up
How to Spot and Avoid Excipient Problems
The problem? You won’t see excipients listed on your pill bottle. They’re not required to be there. So how do you protect yourself? 1. Ask your pharmacist. They have access to the full drug monograph. Ask: “What are the inactive ingredients in this generic?” If they don’t know, ask them to look it up. Most pharmacists can tell you if a generic contains lactose, gluten, or dyes. 2. Check the package insert. It’s usually tucked inside the box. Look for the “Inactive Ingredients” section. If you’re unsure, Google the drug name + “package insert.” 3. Keep a medication diary. Write down when you switch medications and what symptoms you notice. Did your headaches start after switching to the new generic? Did your joint pain get worse? Track it. This helps you and your doctor connect the dots. 4. Stick with the same generic manufacturer. Generic drugs from different companies can have different excipients-even if they’re both labeled the same. If you find a generic that works for you, ask your pharmacist to keep ordering it from the same maker. 5. Ask your doctor to write “Dispense as Written” or “Do Not Substitute.” This legally prevents the pharmacy from switching your medication without your doctor’s approval. It’s your right.Why Don’t Generic Manufacturers Use the Same Excipients?
You might wonder: why not just copy the brand’s formula exactly? The answer is cost and patent avoidance. Excipients are often protected by their own patents or proprietary blends. Generic makers don’t need to copy them-they just need to prove their version works. So they choose cheaper, available ingredients that meet FDA standards. That’s fine for most people. But for those with sensitivities, it’s like being handed a new car with the same engine but different tires, brakes, and suspension. The car moves. But if you’re used to the original ride, you might feel every bump.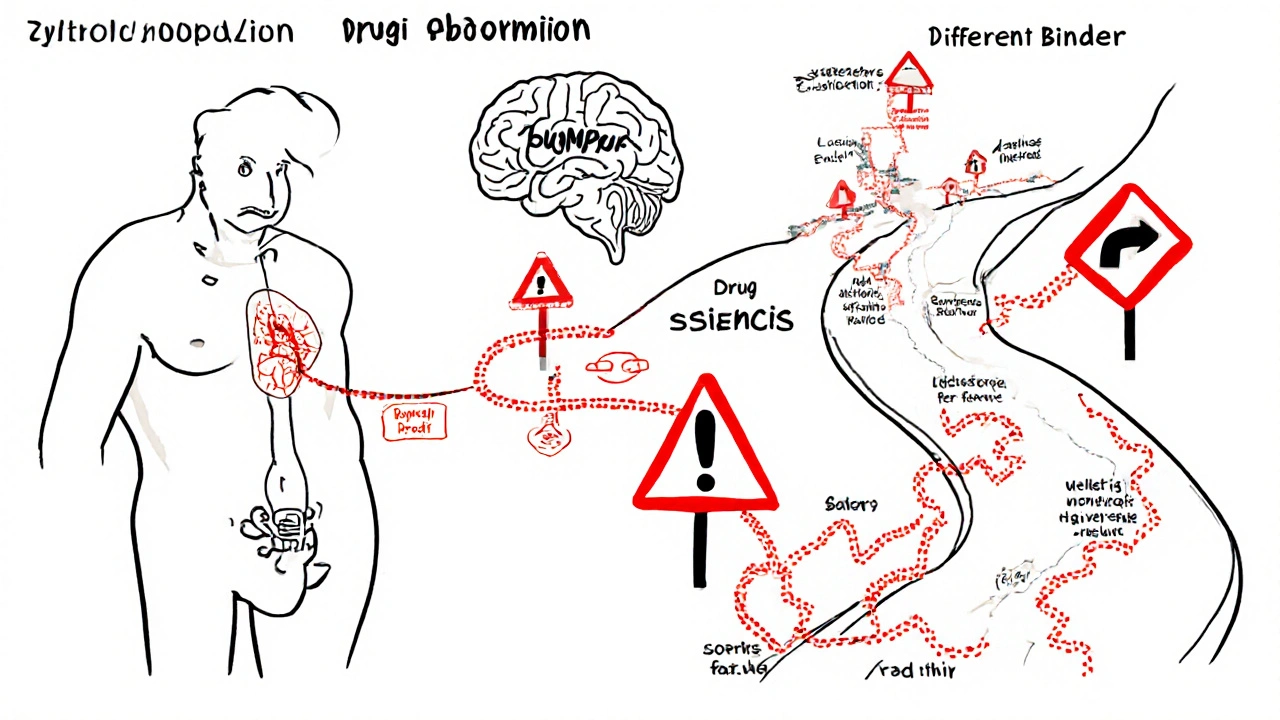
What’s Changing?
The system is slowly catching up. In 2024, the FDA announced plans to create a public database listing excipients in both brand and generic drugs. That’s a big step. Right now, you have to dig to find this info. Soon, it might be as easy as checking a website. Some generic manufacturers are already responding. In early 2024, major companies began voluntarily standardizing excipients in high-risk drugs like levothyroxine and warfarin. One company even started marketing a “clean excipient” line-no dyes, no lactose, no controversial fillers-for patients with sensitivities. And research is catching up too. A March 2024 study found that 68% of adverse events from generic switches could have been predicted if patients were screened for excipient intolerances before switching.Is It Worth Paying More for the Brand?
Cost matters. Generics save the U.S. healthcare system over $370 billion a year. For most people, the savings are worth it. But if you’ve had a bad reaction, or you’re on a narrow therapeutic index drug, paying more for the brand might be the smarter, safer choice. Medicare Part D plans charge $1-$5 co-pays for generics versus $40-$100 for brands. But if you’re spending $200 a month on emergency room visits because your generic made you sick, the math changes. Talk to your doctor. Ask: “Is this a drug where small changes in absorption could hurt me?” If the answer is yes, and you’ve had issues before, ask for the brand. Most insurers will approve it if your doctor documents a medical necessity.Bottom Line: Know Your Meds
Generic drugs are safe, effective, and essential for affordable healthcare. But they’re not always identical. Excipients-the invisible ingredients-can cause real side effects in sensitive people. You don’t need to avoid generics. But you do need to be informed. Don’t assume your new pill is the same as the old one. Ask questions. Track your symptoms. Know your intolerances. And if something feels off after a switch-don’t brush it off. It might not be in your head. It might be in the filler.Can generic medications cause allergic reactions?
Yes. While the active ingredient is the same, excipients like lactose, dyes, or preservatives in generics can trigger allergies or intolerances. For example, a patient allergic to FD&C Red No. 40 might react to a generic version of a blood pressure pill that uses that dye, even if the brand version doesn’t. Always check inactive ingredients if you have known allergies.
Why do some people feel worse on generic thyroid medication?
Thyroid meds like levothyroxine have a narrow therapeutic index. Small changes in how quickly the drug is absorbed-caused by different fillers or coatings in generics-can lead to under- or over-treatment. Patients may feel fatigued, gain weight, or develop heart palpitations. Consistency in the manufacturer and formulation is key. If you switch and feel off, get your TSH levels checked.
How do I find out what excipients are in my medication?
Check the package insert that comes with your prescription. If you don’t have it, ask your pharmacist for the drug’s full prescribing information. You can also search online for “[drug name] package insert” and look for the “Inactive Ingredients” section. The FDA’s upcoming public database will make this easier in the future.
Can I ask my doctor to only prescribe brand-name drugs?
Yes. Your doctor can write “Dispense As Written” or “Do Not Substitute” on your prescription. This legally prevents the pharmacy from switching to a generic without your doctor’s approval. Insurers may require documentation of prior adverse reactions to generics before approving the brand, so keep records of any side effects.
Are all generic drugs the same?
No. Different manufacturers use different excipients, coatings, and manufacturing processes. Two generics of the same drug can behave differently in your body. If you find a generic that works for you, stick with the same manufacturer. Switching between generic brands can trigger side effects-even if both are labeled the same.
Is there a list of excipients that commonly cause problems?
Yes. Common culprits include lactose (for lactose-intolerant people), gluten (for celiac patients), dyes like FD&C Red No. 40 or Yellow No. 5 (for those with dye allergies), and preservatives like parabens or sulfites. If you have known sensitivities, always verify these ingredients before accepting a new generic version.
Next time you pick up a prescription, don’t just take the pill. Ask: What’s in it? Who made it? And why? Your body might thank you.








14 Comments