Biosimilars are highly similar, lower-cost versions of complex biologic drugs. They offer proven safety and effectiveness with 15-30% savings, helping patients access treatments for cancer, arthritis, and autoimmune diseases without sacrificing quality.
Biosimilar Savings: How Generic Biologics Cut Drug Costs Without Compromising Care
When you hear biosimilar savings, cost-reducing alternatives to brand-name biologic drugs that work the same way but cost far less. Also known as generic biologics, they're not just cheaper—they're changing who can afford treatments for cancer, rheumatoid arthritis, diabetes, and more. Unlike regular generics, which copy small-molecule pills, biosimilars are complex proteins made from living cells. They don’t match the original drug molecule-for-molecule, but they’re proven to have no meaningful difference in safety or effectiveness. The FDA and Health Canada approve them only after rigorous testing—so you’re not trading quality for price.
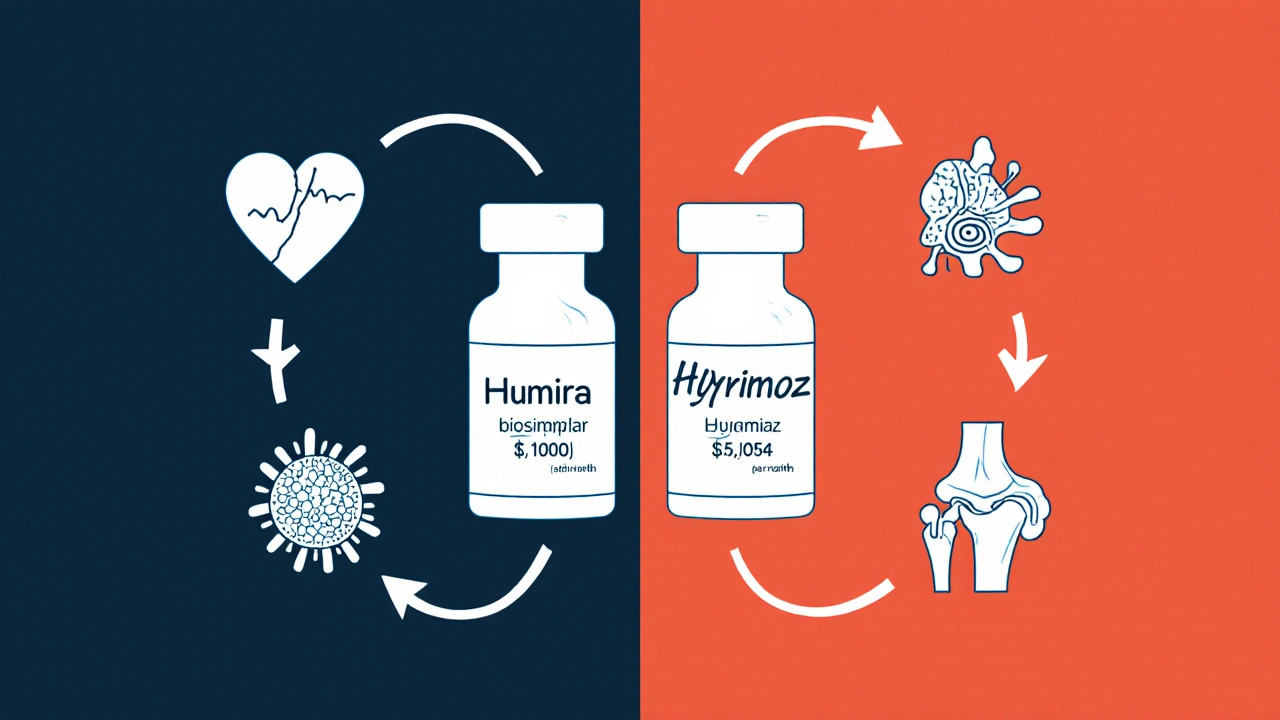
Why does this matter? Brand-name biologics like Humira, Enbrel, or Herceptin can cost over $20,000 a year. Biosimilars slash that by 15% to 85%, depending on the drug and where you live. For someone on insulin or a rheumatology drug, that’s not a minor discount—it’s the difference between taking your medicine or skipping doses. And it’s not just individuals saving. Hospitals, insurers, and government programs are switching to biosimilars to stretch budgets without hurting outcomes. In Canada, where drug pricing is tightly regulated, biosimilar adoption has grown fast because the system rewards real savings.
But here’s the catch: not all biosimilars are created equal in how they’re used. Some require special handling or different injection devices. Others only work for certain conditions covered by the original drug. That’s why switching isn’t always automatic—your doctor needs to confirm it’s safe for you. Still, when it works, the results are clear: more people get treated, fewer go broke, and the system keeps running. You’ll find posts here that break down real cases—like how a biosimilar version of adalimumab helped a patient cut their monthly cost from $3,000 to $400, or why some people still get confused between biosimilars and generics. You’ll also see how insurance rules, pharmacy substitutions, and even patient education play into whether these savings actually reach you.
What you’ll see below isn’t theory. It’s real stories, real data, and real choices people are making every day to save money on high-cost drugs. Whether you’re managing a chronic condition, helping a parent navigate prescriptions, or just trying to understand why your co-pay dropped last month, the articles here give you the facts without the fluff.