Biosimilars are highly similar, lower-cost versions of complex biologic drugs. They offer proven safety and effectiveness with 15-30% savings, helping patients access treatments for cancer, arthritis, and autoimmune diseases without sacrificing quality.
Biosimilars: What They Are, How They Work, and Why They Matter
When you hear biosimilars, highly similar versions of complex biologic drugs that are made after the original patent expires. Also known as biologic generics, they offer the same clinical benefits as the original drug but at a fraction of the cost. Unlike regular generics, which are simple chemical copies, biosimilars are made from living cells — think proteins, antibodies, or hormones — and are far more complex to produce. That’s why they’re not exact copies, but close enough to work the same way in your body, with no meaningful difference in safety or effectiveness.
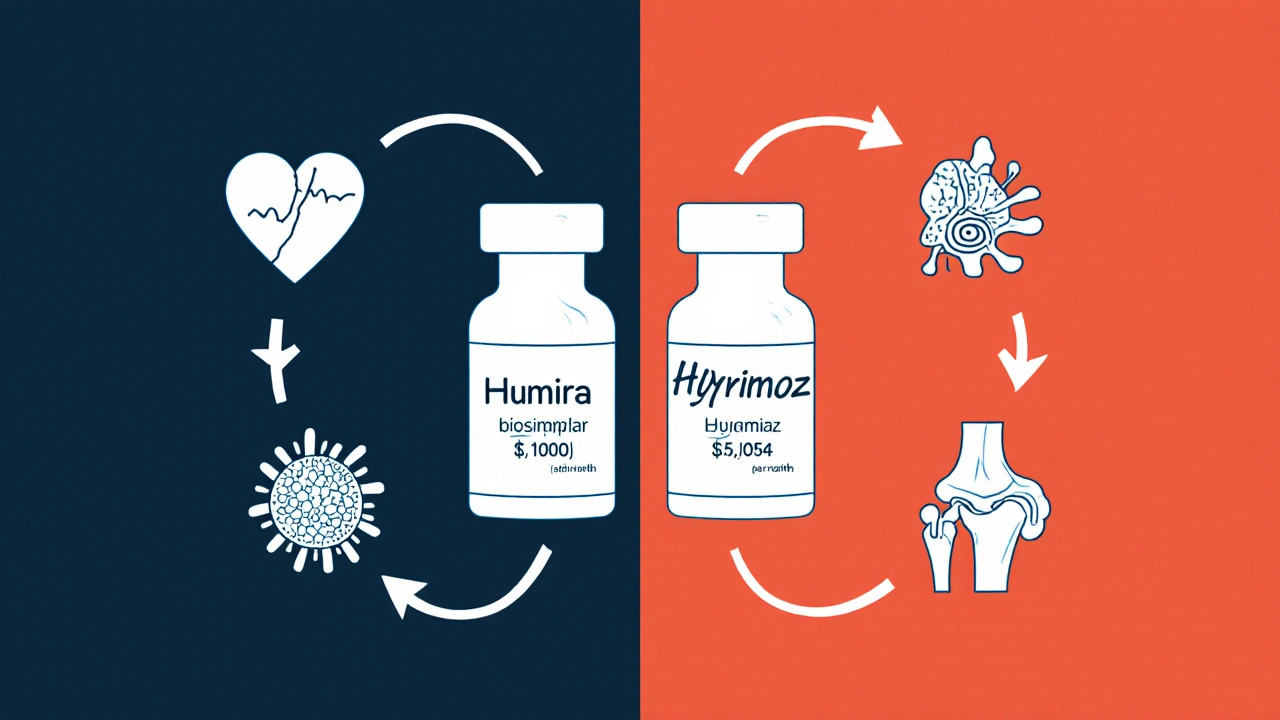
These drugs are changing how people treat chronic conditions like rheumatoid arthritis, Crohn’s disease, and certain cancers. For example, a biosimilar to adalimumab (Humira) can cost 30-70% less, making treatment possible for people who couldn’t afford it before. But they’re not interchangeable with the original without a doctor’s approval. Why? Because even tiny differences in how they’re made can affect how your body reacts — especially if you’re on a narrow therapeutic index drug. That’s why generic medications, simple chemical copies of small-molecule drugs. Also known as brand-name equivalents, they work differently than biosimilars. You can swap generics like metformin or lisinopril without worry. Biosimilars? That’s a conversation with your provider.
Many people worry that biosimilars are "second-rate." But the FDA requires them to meet the same strict standards as the original. Clinical trials prove they work just as well. The difference isn’t in quality — it’s in cost and access. And that’s why more insurers are pushing for biosimilars: they save billions without sacrificing outcomes. But here’s the catch: not all biosimilars are created equal. Some work better for certain patients, and switching from the original drug can sometimes trigger unexpected side effects. That’s why your doctor needs to monitor you closely, especially if you’re switching from a biologic like etanercept or infliximab.
What you’ll find in this collection isn’t just theory. It’s real-world guidance from people who’ve switched, doctors who’ve prescribed, and patients who’ve seen the difference. You’ll read about how drug cost savings, the financial benefit patients gain when using lower-priced alternatives to expensive biologics. Also known as medication affordability, they impact daily life, why some pharmacies hesitate to stock them, and how to tell if a biosimilar is right for you. You’ll also see how they stack up against other alternatives — from older generics to newer targeted therapies. No fluff. No marketing. Just what you need to know to make smart, informed choices about your treatment.