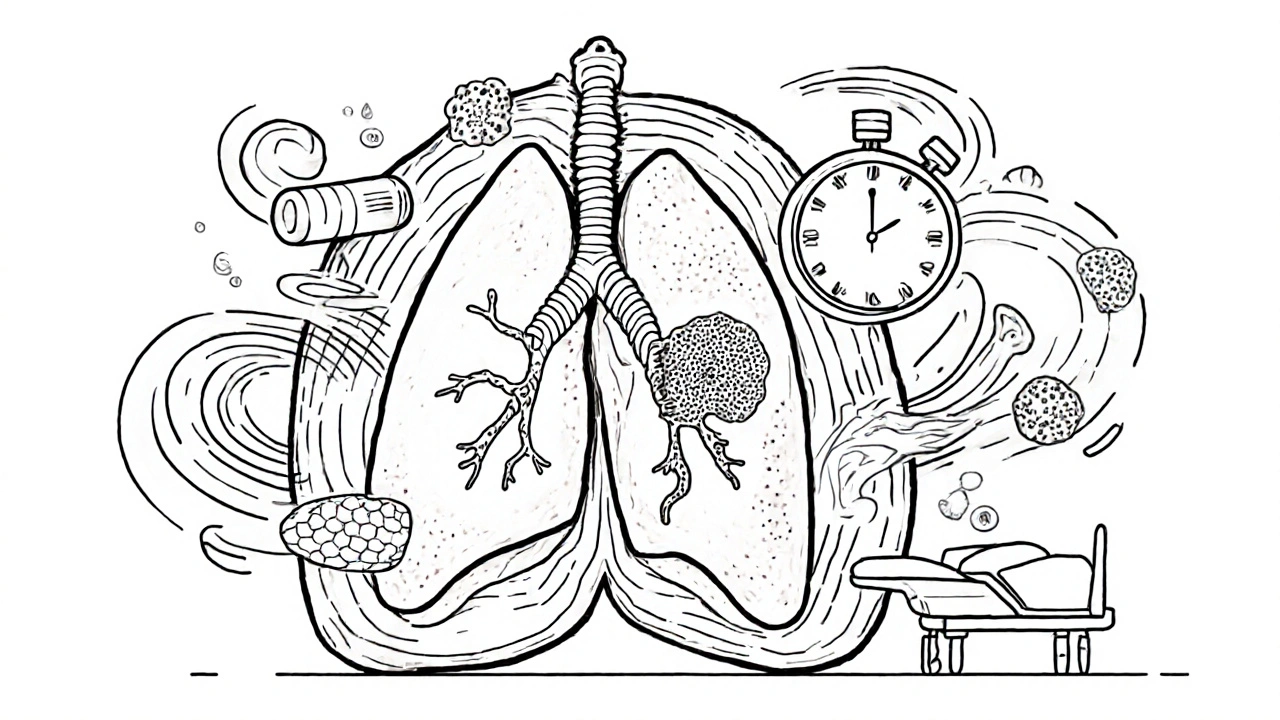
Neoadjuvant therapy treats cancer before surgery to shrink tumors and test drug effectiveness, while adjuvant therapy clears leftover cells after. New evidence shows neoadjuvant-only may be just as effective with fewer side effects, especially for lung and breast cancer.
Cancer Treatment Sequencing: What Works When and Why
When you hear cancer treatment sequencing, the planned order of therapies like chemotherapy, immunotherapy, and targeted drugs used to fight cancer. Also known as treatment algorithm, it's not just about what drugs to use—it's about when to use them, and why one comes before another. This isn’t random. Doctors follow evidence-based paths shaped by cancer type, stage, genetics, and how your body responds.
For example, in advanced lung cancer, targeted therapy, drugs that attack specific mutations like EGFR or ALK in cancer cells often comes first if your tumor has those markers. But if no mutation is found, immunotherapy, treatments that help your immune system recognize and destroy cancer cells might be the starting point. And if those don’t work—or if the cancer is aggressive—chemotherapy, drugs that kill fast-growing cells, both cancerous and healthy still plays a key role, often after other options are tried.
The sequence matters because some treatments make others more effective. Giving immunotherapy before chemo can sometimes boost immune response. Using a targeted drug first might shrink tumors enough to make surgery possible. But if you use the wrong drug too early, you could lose the chance to use it later when it’s most needed. That’s why genetic testing, tumor biopsies, and ongoing monitoring are part of every sequencing decision.
It’s not just about drugs either. Radiation, surgery, and even clinical trials can be part of the sequence. A patient with breast cancer might get neoadjuvant chemo to shrink a tumor before surgery, then follow up with hormone therapy and radiation. Someone with melanoma might start with immunotherapy, switch to targeted therapy after resistance develops, and then try a new combination in a trial. Each path is unique.
What you’ll find in the posts below aren’t just lists of drugs. They’re real-world examples of how treatment sequencing plays out in practice—what works, what doesn’t, and why doctors make the choices they do. You’ll see how side effects, cost, and patient health shape the plan. No theory. No fluff. Just what matters when you’re trying to outsmart cancer one step at a time.