COPD Inhalers: Types, Uses, and What You Need to Know
When you have COPD inhalers, devices used to deliver medication directly to the lungs for chronic obstructive pulmonary disease. These are not just tools—they’re lifelines for millions who struggle to breathe every day. COPD, or chronic obstructive pulmonary disease, makes it hard to get air in and out of your lungs. That’s where inhalers come in. They put the medicine exactly where it’s needed: deep in your airways. No pills, no shots—just a puff that helps you breathe easier.
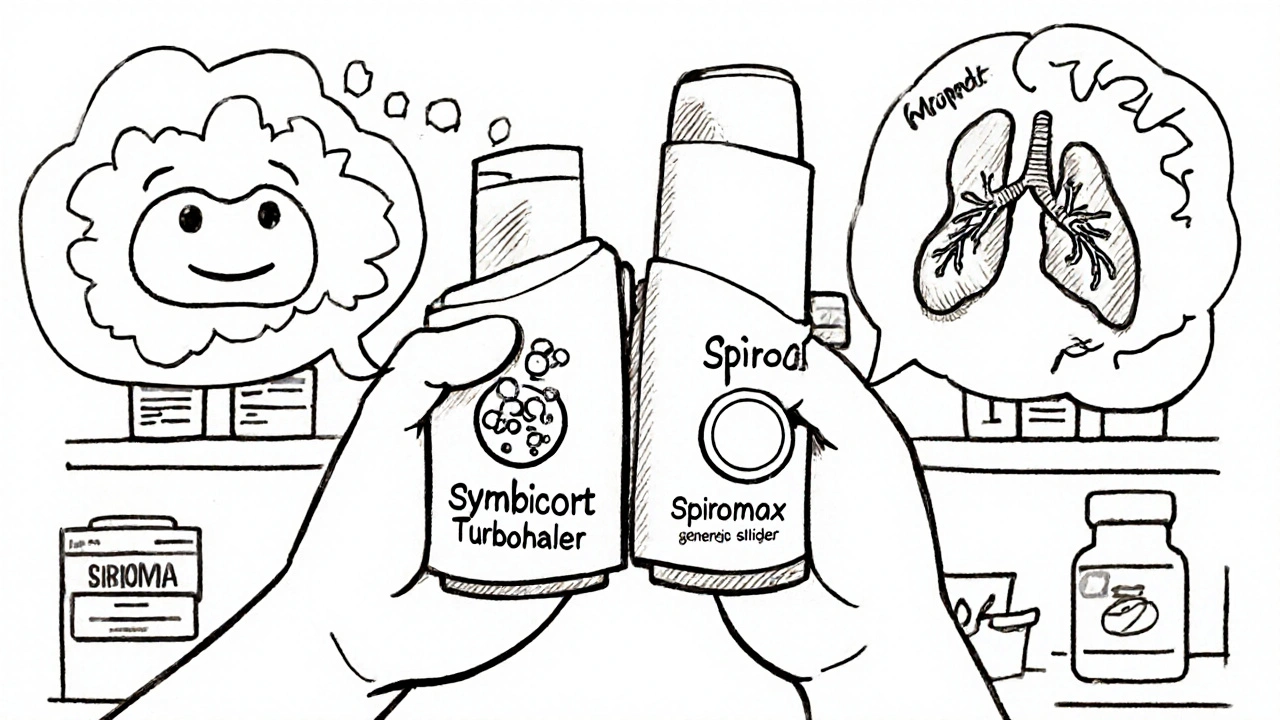
There are two main kinds of COPD inhalers: bronchodilators, medications that relax the muscles around your airways to open them up and corticosteroid inhalers, anti-inflammatory drugs that reduce swelling and mucus in the lungs. Bronchodilators like albuterol or tiotropium give quick relief when you’re short of breath. Corticosteroids like fluticasone or budesonide are for daily use to prevent flare-ups. Some inhalers combine both types—this is common for people with moderate to severe COPD who need more control.
It’s not just about picking the right inhaler. How you use it matters just as much. If you don’t coordinate your breath with the puff, most of the medicine ends up in your mouth, not your lungs. That’s why many people need spacers—small plastic tubes that help the medicine reach deeper. And if you’re using a dry powder inhaler, you have to inhale fast and hard. Mistakes here mean less relief and more trips to the doctor.
Side effects are usually mild—dry mouth, throat irritation, or a hoarse voice—but they add up over time. Rinsing your mouth after each use cuts down on yeast infections and hoarseness. It’s simple, but it makes a real difference. And while inhalers don’t cure COPD, they keep you moving, sleeping, and doing the things you care about.
You’ll also see people talking about rescue inhalers versus maintenance inhalers. Rescue ones are for sudden symptoms—like when you’re out walking and suddenly can’t catch your breath. Maintenance ones are for daily use, even when you feel fine. Skipping them because you’re not coughing or wheezing is a common mistake. COPD doesn’t take days off, and neither should your treatment.
What’s in your inhaler affects your whole life. It’s not just about the drug inside—it’s about how it fits into your routine, your budget, and your daily rhythm. Some people need multiple devices. Others get by with one. The right setup depends on your symptoms, your lung function, and what your body responds to.
Below, you’ll find real-world insights from people managing COPD every day. From how to save money on prescriptions to understanding why one inhaler works for your neighbor but not you, these posts cut through the noise. You’ll see what actually helps—and what doesn’t—based on real experiences and current medical advice. No fluff. Just what you need to take control of your breathing.