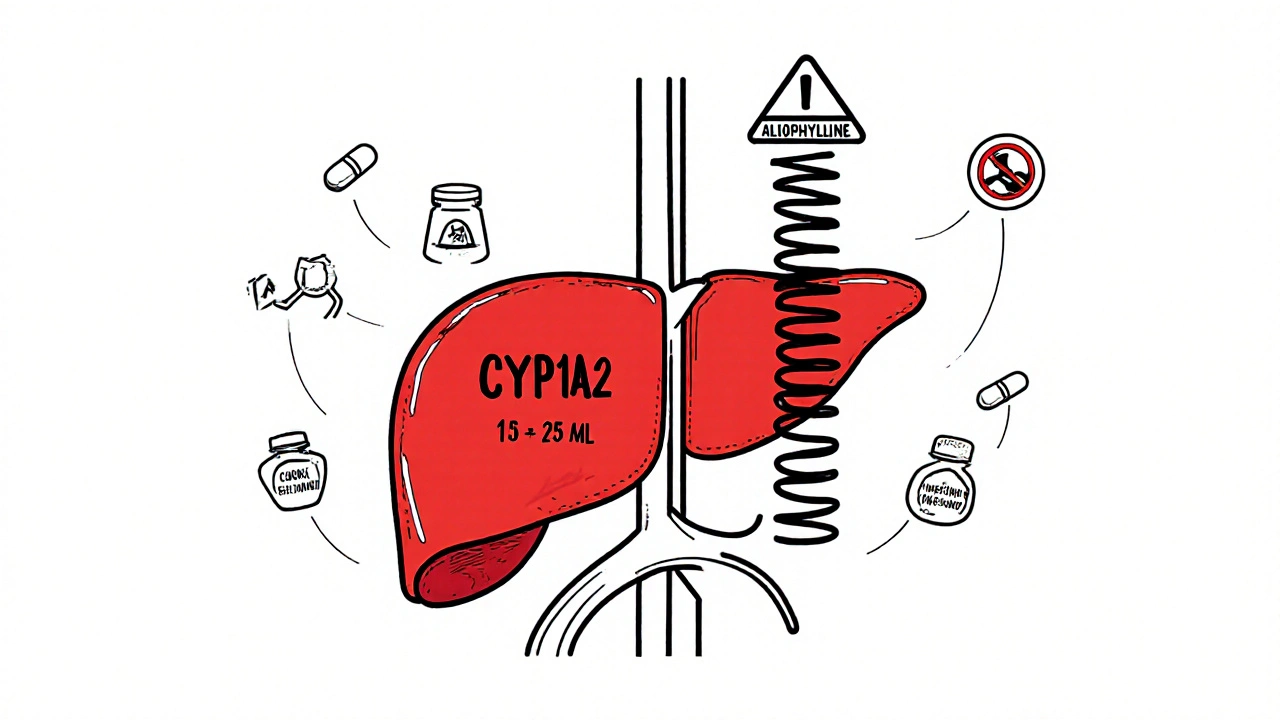
Theophylline has a narrow therapeutic window, and common medications like cimetidine, fluvoxamine, and allopurinol can dangerously reduce its clearance, leading to life-threatening toxicity. Know the risks and how to prevent them.
CYP1A2 Inhibitors: What They Are and How They Affect Your Medications
When you take a medication, your body doesn’t just absorb it and call it a day—it CYP1A2 inhibitors, substances that block the CYP1A2 liver enzyme responsible for breaking down many drugs. Also known as cytochrome P450 1A2 inhibitors, these compounds slow down how quickly your liver clears certain medicines from your system, which can lead to higher drug levels and unexpected side effects. This isn’t theoretical. If you’re on a drug like clozapine or theophylline, and you start drinking large amounts of grapefruit juice or taking fluvoxamine, your body can’t process those meds the way it used to. That’s not a coincidence—it’s biology.
The liver uses enzymes like CYP1A2 as its main cleanup crew. When you take something that blocks this enzyme—like some antidepressants, antibiotics, or even herbal supplements—you’re essentially putting a wrench in the system. Common CYP1A2 inhibitors include fluvoxamine, an antidepressant that strongly interferes with this enzyme, ciprofloxacin, a widely used antibiotic that can raise levels of caffeine and other drugs, and even green tea extract, a supplement that can alter how your body handles medications. You might not think of green tea as a drug, but its active compound, EGCG, acts like a silent gatekeeper in your liver. That’s why some people suddenly feel jittery after switching to green tea pills, even if they’ve always tolerated caffeine fine.
It’s not just about what you take—it’s about what you’re already on. People on antipsychotics, asthma meds, or blood thinners are especially at risk because these drugs are metabolized heavily by CYP1A2. If your doctor doesn’t know you’re taking a new supplement or changing your coffee habit, you could be walking into a hidden interaction. This is why so many of the articles here focus on real-world medication conflicts: from how green tea extract messes with statins, to how diet affects antidepressants like doxepin, to why switching generics can cause problems due to inactive ingredients. These aren’t edge cases—they’re everyday risks.
You don’t need to be a scientist to stay safe. Just know this: if you’re on any regular medication and you start something new—a supplement, a new coffee routine, or even a different brand of tea—you should check whether it affects CYP1A2. The list below includes real stories from people who ran into trouble, how they figured it out, and what they did next. These aren’t theory papers. These are practical fixes from real patients and doctors who’ve seen the fallout when enzyme interactions go ignored.