Why your generic medication might cost more than the brand name - it's not about quality, it's about insurance deals. Learn how tiered copays work and what you can do to save money.
Generic Drug Copay: What It Really Costs and How to Save
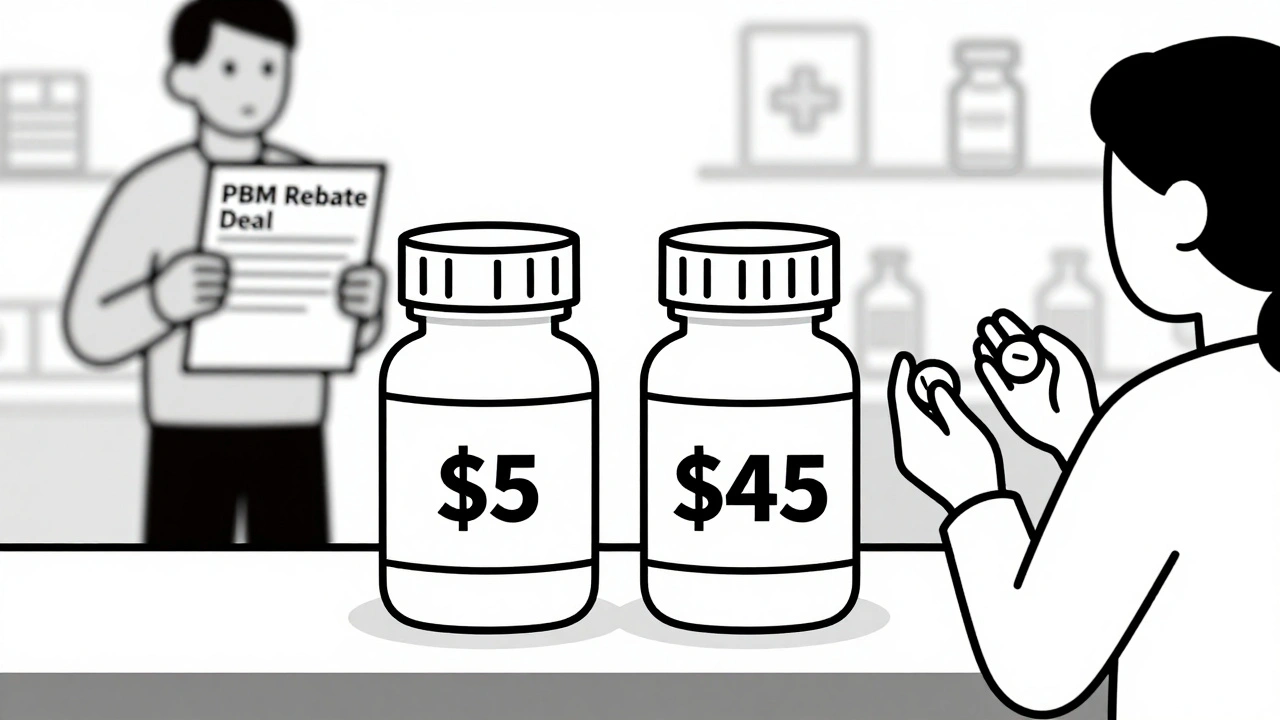
When you pick up a generic drug copay, the fixed amount you pay for a generic medication under your insurance plan. Also known as a prescription copayment, it’s often the only part of your drug cost you see at the pharmacy counter—but it’s not the whole story. Many people assume generic drugs mean cheap drugs, and that’s mostly true. But the copay you pay? That’s set by your insurer, not the drugmaker. And it can jump from $5 to $50 depending on your plan, your state, or even the pharmacy you use.
Not all generic drugs are treated the same. Your insurance plan puts them into formulary tiers, categories that determine how much you pay for each type of medication. Tier 1 usually means the cheapest generics—like metformin or lisinopril—with copays as low as $3. Tier 3 or 4? That’s where you might pay $20 or more, even for a generic. Why? Because some generics are newer, less commonly used, or your insurer has a deal with a specific brand. This isn’t about effectiveness—it’s about contracts. And if your doctor prescribes a drug that’s not on your plan’s preferred list, you might get stuck with a higher copay… unless you ask for a prior authorization or switch.
Here’s what most people don’t realize: your insurance copay, the amount you pay out of pocket for covered prescriptions. isn’t always the lowest price you can get. Sometimes, paying cash for a generic drug costs less than using your insurance. A 30-day supply of atorvastatin? $10 cash at Walmart. With insurance? $18 after your $15 copay. That’s because insurers negotiate bulk rates with pharmacies, but those deals don’t always pass savings to you. Always ask your pharmacist: "Is this cheaper without my insurance?" It’s a simple question that can save you hundreds a year.
Then there’s the push for generic substitution, when a pharmacist swaps a brand-name drug for a cheaper generic version. It’s legal, common, and usually safe. But not always smooth. Some patients report side effects after switching—dry mouth from a new generic anticholinergic, dizziness from a different formulation of lisinopril-HCTZ. That’s not the generic’s fault. It’s about how your body reacts to fillers, binders, or slight differences in absorption. If you notice a change after a switch, tell your doctor. You’re not being difficult—you’re being informed.
And don’t forget: if your copay is too high, help exists. community clinics, local health centers that offer low-cost or free medications to uninsured or underinsured patients. often have partnerships with pharmacies to give out generics for $0–$10. Programs like GoodRx, NeedyMeds, or manufacturer coupons can slash prices too. You don’t need a perfect income or perfect insurance to get affordable meds. You just need to ask.
Bottom line: your generic drug copay isn’t fixed, it’s negotiable. It’s not always the best deal, and it’s not always fair. But you have more power than you think. Know your plan’s tiers. Compare cash vs. insurance. Ask about alternatives. And if a switch makes you feel worse—speak up. The system is built to save money, but you’re the one paying the price. Make sure you’re getting real value, not just a lower number on a receipt.
Below, you’ll find real stories and practical guides on how to cut your medication costs, avoid hidden fees, and get the right generics without risking your health. From how insurers force substitutions to how to spot dangerous drug interactions in cheap pills—everything you need to take control of your prescriptions.