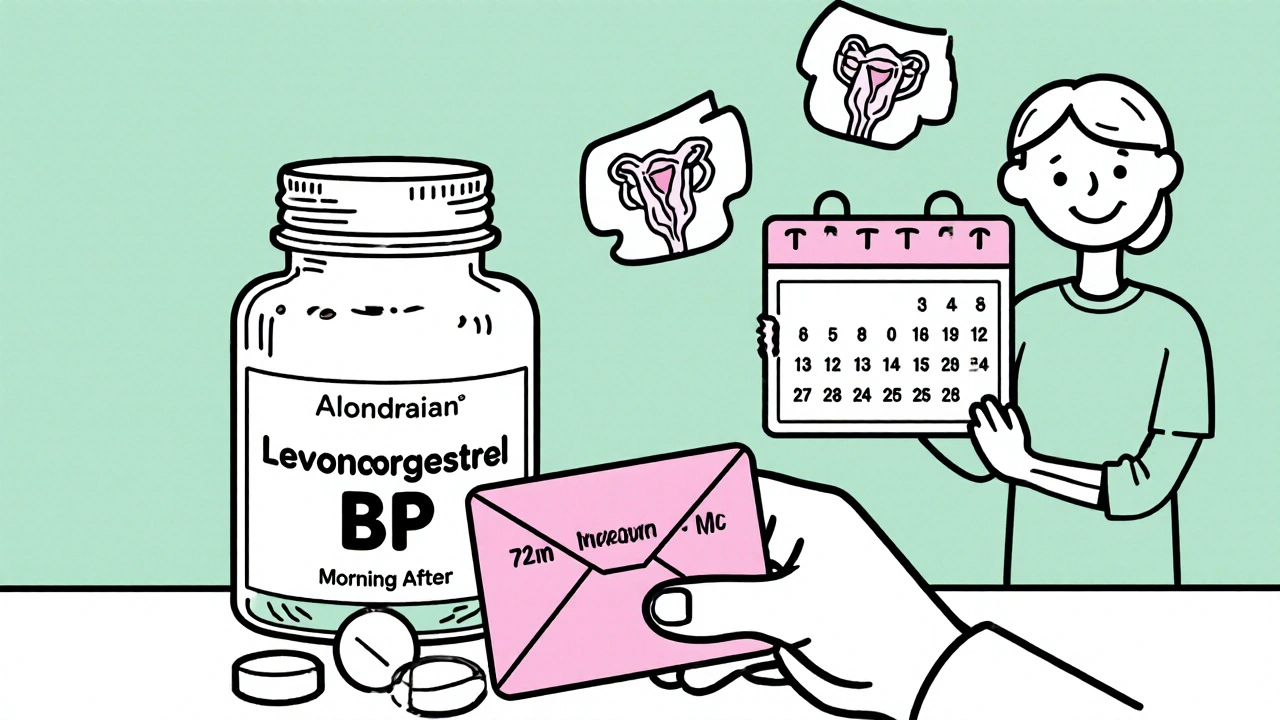
Explore upcoming innovations for levonorgestrel BP, from nanotech and 3D‑printed tablets to personalized dosing and greener manufacturing, and see how they could reshape contraception.
Hormonal Contraception Innovations
When we talk about hormonal contraception innovations, modern methods of birth control that use synthetic hormones to prevent pregnancy with improved safety and convenience. Also known as next-gen birth control, these innovations aren’t just about new pills—they’re about giving people more control, fewer side effects, and longer-lasting options without daily hassle. The old model—take a pill every day at the same time—still works, but it’s no longer the only choice. Today’s options include patches that last a week, implants that last three years, and IUDs that release hormones directly into the uterus, cutting down on systemic exposure and reducing things like mood swings or bloating.
One major shift is in progesterone-only pills, hormonal birth control that contains no estrogen, making them safer for people with high blood pressure, migraines, or a history of blood clots. Also known as the mini-pill, these have been around for decades, but recent versions use lower, more precise doses that are easier to tolerate. Then there’s long-acting reversible contraception, methods like hormonal IUDs and implants that work for years without daily action. Also known as LARCs, these are now recommended as first-line choices by major health groups because they’re more effective than pills and require almost no maintenance. The newer IUDs, like those releasing levonorgestrel, don’t just prevent pregnancy—they also reduce heavy periods and cramps, turning birth control into a multi-benefit tool.
What’s driving these changes? Better science. Researchers now know that not all progesterone types are the same. Some cause less acne or weight gain. Some are designed to stay in the uterus longer, avoiding the liver entirely. There’s even emerging research on low-dose estrogen pills that use novel delivery systems to reduce clotting risks. And for people who hate pills but want flexibility, there are now monthly vaginal rings that release hormones steadily, with fewer spikes than traditional pills.
These innovations aren’t just for young adults. Women in their 40s, people with diabetes, those managing endometriosis—all benefit from tailored hormone options. You don’t have to stick with what your doctor offered ten years ago. The field has moved fast, and the choices now reflect real-world needs: simplicity, safety, and personal fit. Whether you’re looking for something you forget about, something that helps with painful periods, or just something that doesn’t make you feel off, there’s a newer option out there that wasn’t available before.
Below, you’ll find detailed comparisons of the latest hormonal methods, how they stack up against older ones, and what real users report about side effects, cost, and ease of use. No fluff. Just clear, practical insights to help you understand what’s changed—and what actually works today.