Neoadjuvant therapy treats cancer before surgery to shrink tumors and test drug effectiveness, while adjuvant therapy clears leftover cells after. New evidence shows neoadjuvant-only may be just as effective with fewer side effects, especially for lung and breast cancer.
Immunotherapy for Lung Cancer: How It Works and What You Need to Know
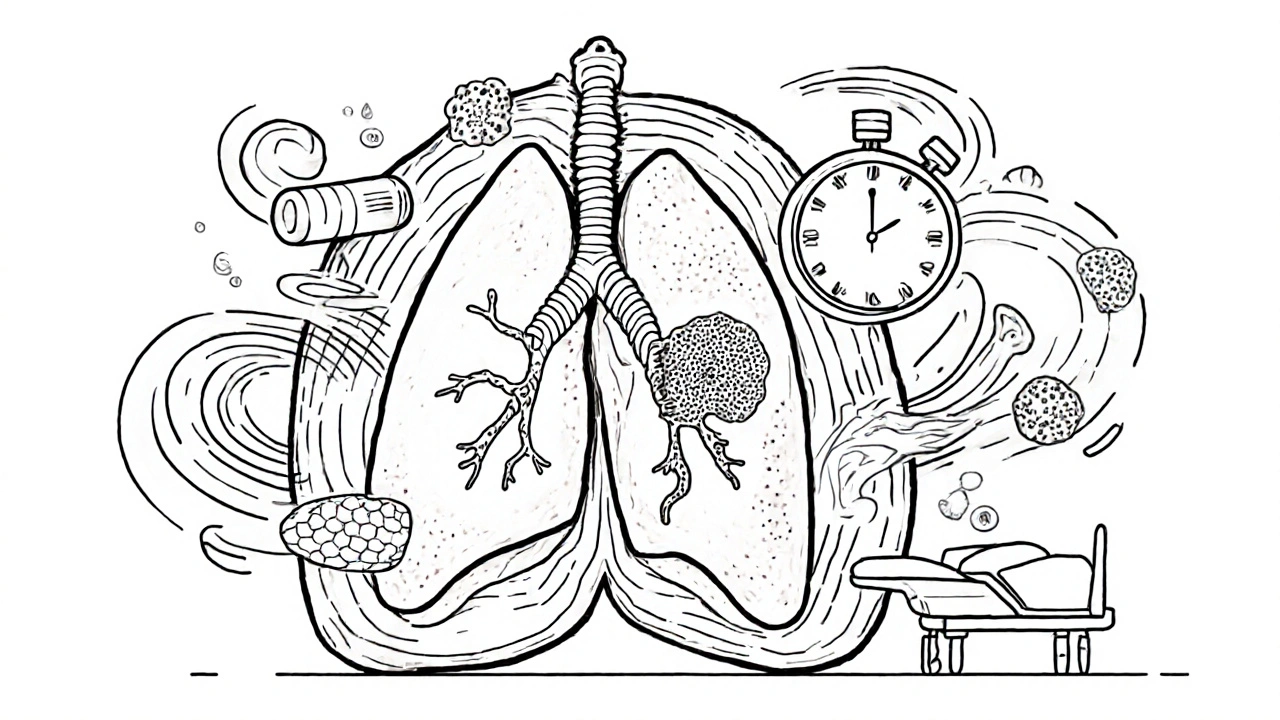
When it comes to treating immunotherapy for lung cancer, a treatment that trains the body’s immune system to recognize and destroy cancer cells. Also known as cancer immunotherapy, it’s changed how doctors approach advanced lung cancer — not by poisoning the body with chemo, but by giving it the tools to fight back on its own. Unlike traditional treatments, immunotherapy doesn’t target the tumor directly. Instead, it removes the brakes that cancer puts on your immune system. This lets T-cells, your body’s natural assassins, find and kill cancer cells they previously ignored.
One of the biggest breakthroughs has been checkpoint inhibitors, drugs that block proteins like PD-1 and PD-L1 that cancer uses to hide from immune cells. These include drugs like Keytruda (pembrolizumab) and Opdivo (nivolumab), which are now standard for many patients with non-small cell lung cancer. They don’t work for everyone — only about 20 to 40% of patients respond — but for those who do, the results can be long-lasting, even years after stopping treatment. Another key player is PD-1 inhibitors, a specific type of checkpoint inhibitor that targets the PD-1 receptor on T-cells. These drugs are often tested first because they tend to have fewer severe side effects than chemo.
What makes immunotherapy different isn’t just how it works — it’s how it feels. Many patients report less nausea, hair loss, or extreme fatigue compared to chemotherapy. But it’s not without risks. Some people develop immune-related side effects: inflammation in the lungs, liver, or even the thyroid. These can be serious, but they’re usually manageable if caught early. That’s why doctors test tumors for biomarkers like PD-L1 expression and tumor mutational burden before starting treatment. These tests help predict who’s most likely to benefit.
You won’t find immunotherapy used alone in early-stage lung cancer — surgery and radiation still lead there. But for stage 3 and 4, it’s often the first line of defense, sometimes combined with chemo or targeted therapy. And while it’s not a cure for everyone, it’s turned what used to be a death sentence into a chronic condition for many. The science is still evolving: new trials are testing combinations, new targets like LAG-3 and TIGIT, and even personalized vaccines made from a patient’s own tumor DNA.
What you’ll find in the articles below isn’t a list of every drug or study — it’s the real-world stuff that matters. How to tell if it’s working. What side effects to watch for. Why some people respond and others don’t. And how to talk to your doctor when the options feel overwhelming. This isn’t theoretical. These are the questions people are asking right now, in clinics and living rooms, while trying to make sense of a diagnosis and a treatment plan that’s unlike anything before it.