Inhaler Device Differences: Which One Works for Your Condition
When you need quick relief from asthma or COPD, the inhaler device, a handheld tool that delivers medication directly to the lungs. Also known as a respiratory inhaler, it’s one of the most common ways to manage chronic lung conditions—but not all inhalers are made alike. The difference between a metered dose inhaler, a pressurized canister that releases a puff of medicine when activated and a dry powder inhaler, a device that releases medication as a fine powder you breathe in isn’t just technical—it affects whether the medicine actually reaches your lungs.
Many people struggle with metered dose inhalers because they require perfect timing: press the canister and breathe in at the same moment. If you’re out of sync, most of the dose hits your throat instead of your airways. Dry powder inhalers don’t need that coordination—they activate when you inhale, making them easier for kids, older adults, or anyone with shaky hands. But they need a strong, fast breath to work. If your lungs are too weak, the powder won’t scatter properly. Then there are soft mist inhalers, newer devices that create a slow-moving cloud of medicine, giving you more time to inhale. Each type has trade-offs: cost, portability, ease of use, and how well it fits your daily routine.
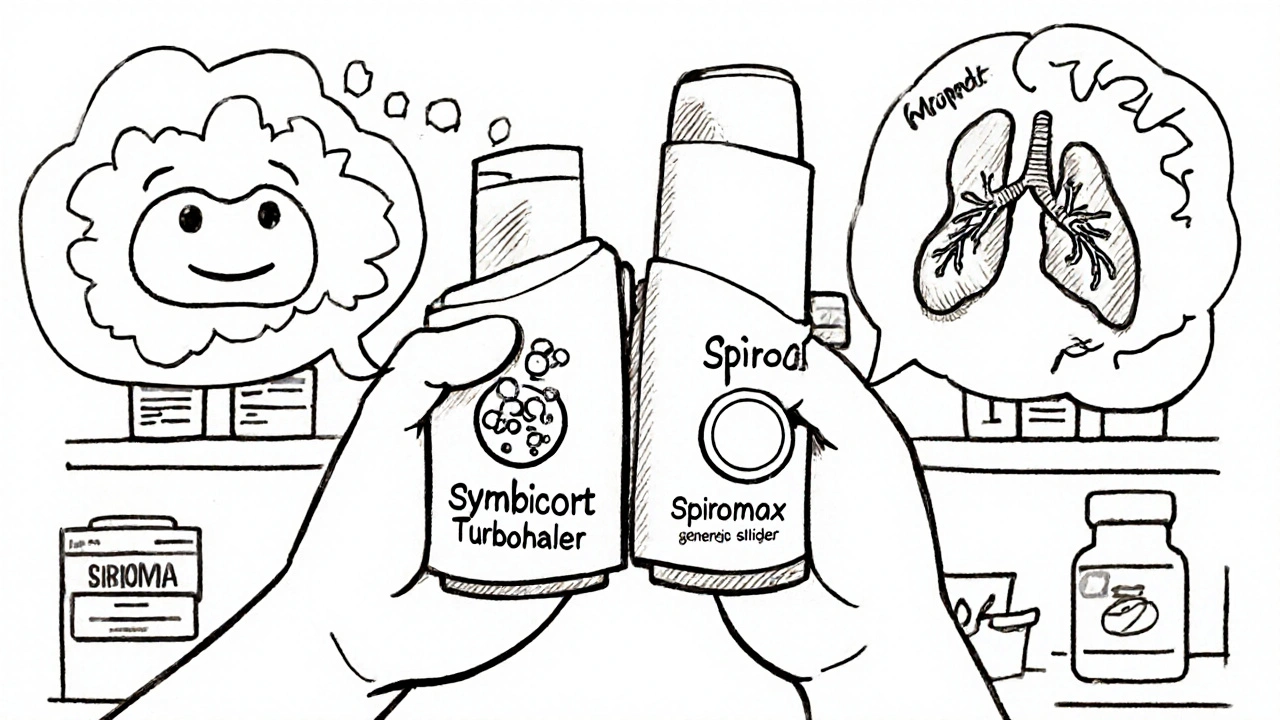
What works for one person might fail for another. Someone with severe COPD might need a dry powder inhaler because they can’t generate enough force for a metered dose inhaler. A child with asthma might do better with a spacer attached to a metered dose inhaler—something that holds the puff so they can breathe in slowly. Even the medication inside matters. Some drugs only come in one type of device. Your doctor doesn’t just pick a brand—they pick a delivery system based on your strength, dexterity, and breathing pattern.
You’ll find posts here that break down exactly how these devices compare: which ones are easiest to use, which ones are most effective for specific conditions, and why some people get no relief even when they think they’re using theirs right. You’ll see real examples of mistakes people make—like not rinsing after steroid inhalers, or assuming all inhalers work the same way. We cover what the research says about adherence, cost differences, and why some patients switch devices mid-treatment. Whether you’re new to inhalers or have been using one for years, the right device can mean fewer flare-ups, less hospital visits, and better control over your breathing.