Learn how to safely take medications with kidney disease. Avoid nephrotoxins, understand eGFR-based dosing, and discover which drugs are safe-or dangerous-for chronic kidney disease.
Kidney Disease Medication Safety: What You Need to Know to Avoid Harm
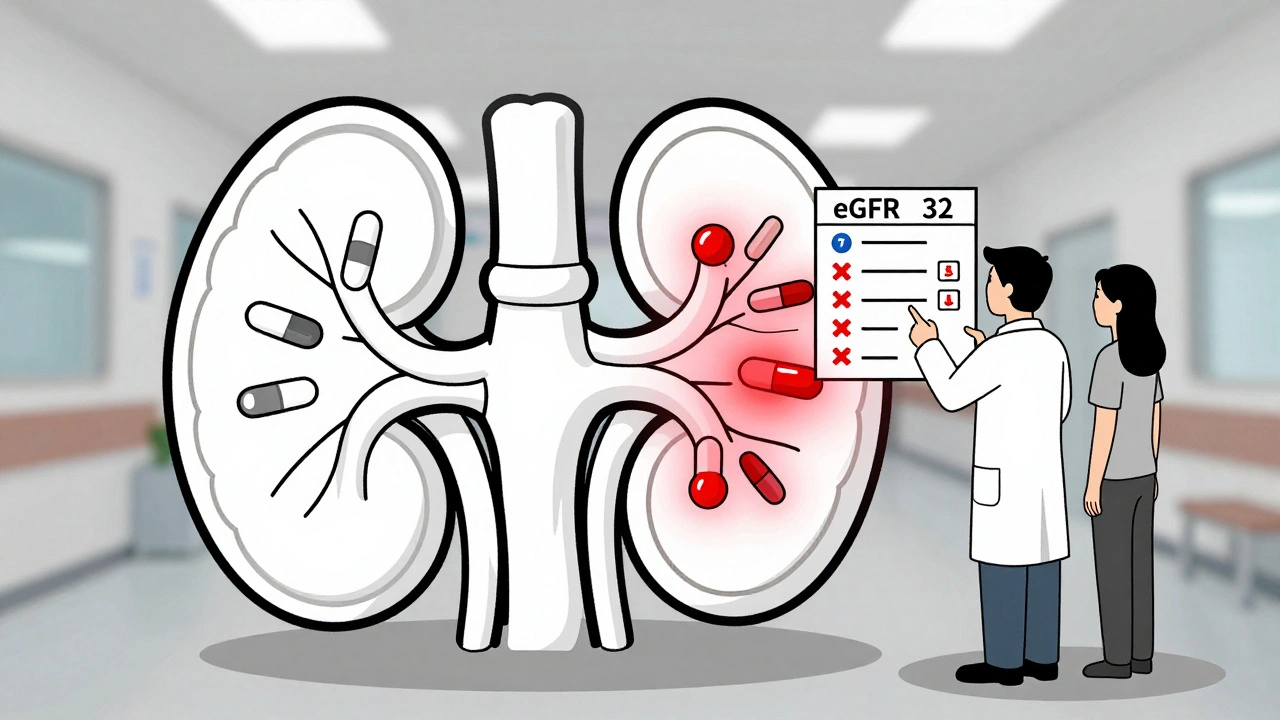
When your kidneys aren't working right, kidney disease medication safety, the practice of using drugs in a way that doesn’t overload or damage weakened kidneys. Also known as renal dosing, it’s not just about taking the right pill—it’s about taking the right amount at the right time. Many common drugs, from painkillers to blood pressure meds, are cleared by the kidneys. If your kidneys are damaged, those drugs build up in your body and can cause toxicity, confusion, or even organ failure. This isn’t theoretical—it’s why hospitals check kidney function before every new prescription.
That’s where renal dosing adjustments, changes in medication dose based on how well your kidneys filter waste. Also known as kidney function dosing, it’s a standard part of care for anyone with chronic kidney disease. A dose that’s safe for a healthy person might be dangerous for someone with CKD. For example, metformin, a common diabetes drug, is often stopped or lowered if kidney function drops below a certain level. Same with NSAIDs like ibuprofen—these can reduce blood flow to the kidneys and make things worse. Even over-the-counter supplements like green tea extract or Diacerein can interfere with kidney function or interact with your meds. And let’s not forget drug interactions, when one medicine changes how another works in your body. Also known as medication interactions, they’re especially risky when kidneys are involved. A drug like cimetidine can slow down the clearance of theophylline, leading to dangerous buildup. Or antibiotics like vancomycin can pile up and damage the kidneys further if dosed too high.
It’s not just about the pills you take—it’s about how you take them. medication adherence, sticking to your prescribed schedule without skipping or doubling up. Also known as treatment compliance, it’s the difference between control and crisis. Missing a dose of a blood pressure med? That spike in pressure can accelerate kidney damage. Taking too much of a diuretic? You could crash your electrolytes. People with kidney disease often juggle multiple meds—sometimes six or more—and it’s easy to get lost. That’s why clear labels, pill organizers, and talking to your pharmacist aren’t luxuries—they’re lifesavers.
What you’ll find below are real, practical guides written for people managing kidney disease—not doctors or researchers. You’ll see how to adjust doses when kidney function changes, which common meds to question, how to spot dangerous interactions, and why skipping a pill isn’t harmless. Whether you’re on dialysis, just diagnosed, or helping a loved one, these posts give you the tools to speak up, ask the right questions, and avoid the hidden dangers most people never even know exist.