When your kidneys aren’t working right, the medicines you take can turn dangerous-even if they’re perfectly safe for someone with healthy kidneys. This isn’t theory. It’s everyday reality for millions. In the U.S. alone, nearly 37 million people live with chronic kidney disease (CKD), and nearly one in three of them ends up in the hospital because of a medication mistake. Most of those cases are preventable. The problem isn’t that doctors are careless. It’s that the rules change when your kidneys slow down, and most people-patients and providers alike-don’t know how.
Why Kidneys Matter for Medications
Your kidneys don’t just make urine. They’re your body’s main filter for drugs. About 70% of all medications rely on your kidneys to get cleared out of your system. When your kidney function drops, those drugs stick around longer. They build up. And that’s when side effects turn into emergencies.Take metformin, the most common diabetes pill. For someone with normal kidneys, it’s safe and effective. But if your eGFR (a measure of kidney function) falls below 30, metformin can cause lactic acidosis-a rare but deadly condition. Even between 30 and 45, you need to be careful. Many patients don’t know this. A 2022 study found that nearly 24% of CKD patients were still getting metformin at unsafe doses because their doctors didn’t adjust it.
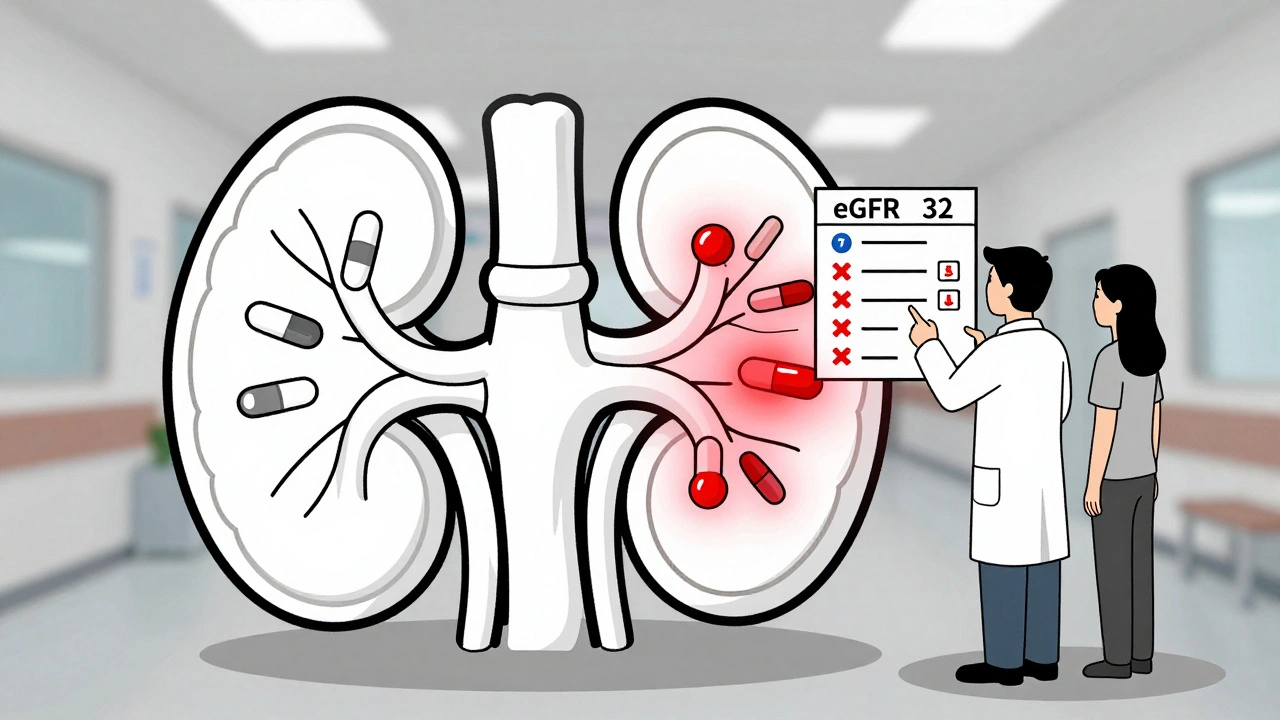
It’s not just diabetes drugs. Antibiotics like gentamicin, painkillers like ibuprofen, and even heart medications like digoxin can become toxic if your kidneys can’t clear them. One Reddit user with stage 4 CKD wrote: "Took two Advil for a headache. Two days later, my creatinine jumped from 3.2 to 5.7. I was hospitalized with acute kidney injury." That’s not an outlier. It’s a pattern.
What Is eGFR? And Why It’s Your Most Important Number
You’ve probably heard the term eGFR. It stands for estimated glomerular filtration rate. It’s a blood test that tells you how well your kidneys are filtering waste. Normal is above 90. Below 60 for three months or more means you have CKD.But here’s the catch: eGFR isn’t static. It can drop fast during illness, dehydration, or after starting a new drug. That’s why checking it once a year isn’t enough. If you have stage 3 or worse CKD, you need it checked every 3 to 6 months. If you’re hospitalized or sick, it should be checked every 24 to 48 hours.
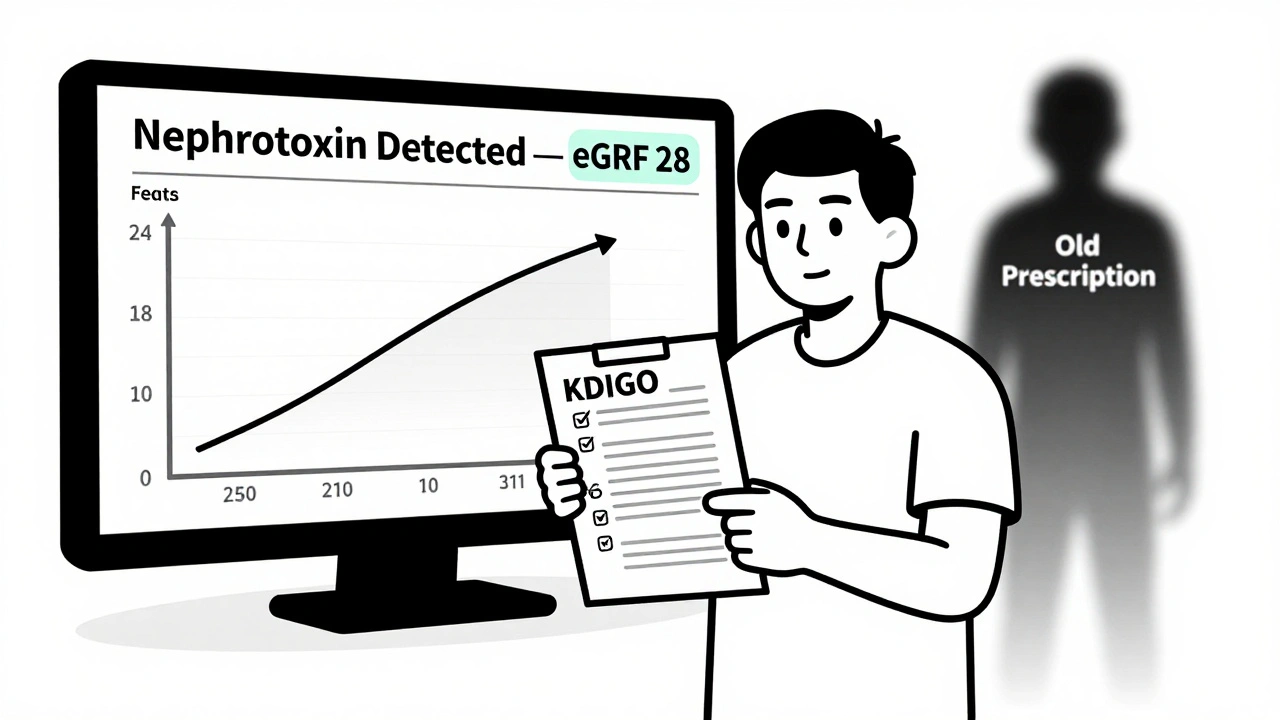
Guidelines from KDIGO (Kidney Disease: Improving Global Outcomes) now say that any time your eGFR drops below 60, you need to review every medication you take. Not just the ones you think are risky. All of them. Even vitamins and over-the-counter stuff.
Most electronic health records still don’t auto-adjust doses based on eGFR. A 2023 study found that 41% of hospitals don’t have protocols for changing drug doses during sudden kidney decline. That means if your eGFR crashes from 50 to 30 in two days, your doctor might not even know you’re at risk-unless you or your pharmacist speak up.
Drugs to Avoid Completely (or Use With Extreme Caution)
Some medications are just too risky for people with kidney disease. Here are the big ones:- NSAIDs (ibuprofen, naproxen, celecoxib): These are the #1 cause of preventable kidney injury in CKD patients. They block blood flow to the kidneys. Even short-term use can cause acute kidney failure. If you need pain relief, use acetaminophen instead-up to 3,000 mg per day.
- Sodium phosphate bowel prep: Used before colonoscopies. Can cause severe, lasting kidney damage. Use polyethylene glycol (PEG) instead. It’s safer and just as effective.
- Contrast dye: Used in CT scans. Can trigger contrast-induced nephropathy. If you need a scan, ask if it’s absolutely necessary. If yes, make sure you’re well-hydrated and your nephrologist is involved.
- Aminoglycosides (gentamicin, tobramycin): Antibiotics that are hard on the kidneys. Dosing must be adjusted based on eGFR and sometimes requires blood level monitoring.
- Metformin: Stop if eGFR is below 30. Reduce dose or hold if between 30-45. Never restart without checking your kidney function again.
And here’s something most people don’t realize: some herbal supplements and weight-loss teas contain aristolochic acid or heavy metals that can destroy your kidneys over time. There’s no regulation. If it’s not FDA-approved, assume it’s risky.

The Game-Changers: Newer Drugs That Are Safe for Kidneys
The good news? Some of the newest medications for diabetes and heart disease are actually protective for kidneys-and they don’t need dose adjustments.SGLT2 inhibitors like dapagliflozin and empagliflozin are a breakthrough. These drugs lower blood sugar, reduce heart failure risk, and slow kidney decline-all without needing to change the dose as your kidney function drops. Even if your eGFR is below 25, you can still take the standard 10 mg dose. That’s unheard of in kidney disease medicine.
The CREDENCE trial showed these drugs cut the risk of kidney failure, dialysis, or death by 39% in people with type 2 diabetes and CKD. Now, KDIGO 2024 recommends them for nearly all CKD patients, even if they don’t have diabetes.
Another newer option is finerenone, a non-steroidal mineralocorticoid receptor antagonist. It’s not a blood pressure pill, but it reduces protein in the urine and protects kidney function when used with ACE inhibitors or ARBs. KDIGO now recommends it if your urine albumin is still high (over 30 mg/g) despite being on maximum-dose ACE/ARB therapy.
And don’t forget GLP-1 receptor agonists like semaglutide and dulaglutide. They’re safe for kidneys, help with weight loss, and reduce heart risk. No dose changes needed.
ACE Inhibitors and ARBs: Don’t Underdose Them
For years, doctors avoided giving full doses of ACE inhibitors (like lisinopril) or ARBs (like losartan) to CKD patients because they saw the creatinine rise and thought it meant harm. That’s wrong.A small rise in creatinine (up to 30%) in the first few weeks is normal. It doesn’t mean the drug is hurting your kidneys-it means it’s working. These drugs reduce pressure inside the kidney’s filtering units, which lowers protein loss and slows disease progression.
KDIGO 2024 calls underdosing these drugs "suboptimal care." The evidence is clear: patients who get the highest tolerated dose have the lowest risk of kidney failure and heart attack. Even if your eGFR is below 30, you can still benefit. The key is to monitor potassium and creatinine closely, not to hold back.
How to Stay Safe: A Practical Checklist
You don’t need to memorize every drug interaction. But you can build a system that keeps you safe:- Know your eGFR. Get it checked every 3-6 months. If you’re sick or hospitalized, ask for it before any new medication is given.
- Keep a current list of every pill, supplement, and OTC drug you take. Include dosages and why you take them.
- Use one pharmacy. A single pharmacy can flag dangerous interactions. NIDDK found that patients using one pharmacy had 42% fewer medication-related kidney injuries.
- Ask your pharmacist. Pharmacists are trained in renal dosing. Ask: "Is this safe for my kidneys? Does it need a dose change?"
- Get a quarterly medication review. Especially if you see multiple doctors. A nephrologist or clinical pharmacist should review your list every 3 months.
- Use a renal dosing app. Apps like Epocrates Renal Dosing or Medscape Renal Dosing are used by 63% of U.S. nephrologists. They’re free and easy to use.
What Happens If You Get It Wrong?
The cost of a medication error in CKD isn’t just medical. It’s financial, emotional, and life-changing.One patient in Australia told her nephrologist: "I took meloxicam for arthritis for six months. I didn’t know it was bad for kidneys. When I got my blood test, my eGFR had dropped from 45 to 28. I needed dialysis within a year."
That’s not rare. In the U.S., medication-related kidney injuries account for 28% of all CKD hospitalizations. Many of these patients end up on dialysis earlier than they should have. And once you start dialysis, your life changes forever.
But the reverse is also true. A patient on DaVita’s forum wrote: "My nephrologist used the KDIGO checklist. She caught that my metformin dose was too high when my eGFR dropped to 38. We switched me to a safer drug. I’ve been off dialysis for 3 years now."
That’s the difference between ignorance and awareness.
The Future: Better Tools, Better Outcomes
Change is coming. The FDA is updating its guidance in 2026 to require real-world data on how drugs behave in people with kidney disease. That means future drug labels will be more accurate.Some hospitals are now using AI-powered alerts that pop up in electronic records when a doctor tries to prescribe a nephrotoxic drug to a CKD patient. The Veterans Health Administration saw a 37% drop in inappropriate dosing after they rolled out these alerts in 2019.
And in 2026, KDIGO will release a standardized medication safety checklist for CKD patients. It’ll be simple: a one-page form you can bring to every appointment. No more guessing. Just check, ask, adjust.
For now, the best tool you have is knowledge. And the best ally you can have is your pharmacist.
Can I still take ibuprofen if I have kidney disease?
No, it’s not safe. Ibuprofen and other NSAIDs reduce blood flow to the kidneys and can cause sudden kidney injury, especially in people with CKD. Even occasional use can spike creatinine levels. Use acetaminophen (Tylenol) instead, but don’t exceed 3,000 mg per day. Always check with your doctor before taking any pain reliever.
Is metformin always dangerous for kidney disease patients?
Not always. Metformin is safe for people with eGFR above 45. Between 30 and 45, you can still take it but at a lower dose and with close monitoring. Below 30, it’s contraindicated because of the risk of lactic acidosis. Many patients stop metformin too early, missing out on its benefits. Work with your doctor to adjust the dose based on your current kidney function-not a past number.
Do all blood pressure medications need dose changes in kidney disease?
No. ACE inhibitors and ARBs are actually recommended at full doses in CKD because they protect the kidneys. But other blood pressure drugs like diuretics or beta-blockers may need adjustments. Always check each medication individually. SGLT2 inhibitors like dapagliflozin are now considered blood pressure-friendly and kidney-protective with no dose changes needed.
What should I do before a CT scan with contrast dye?
Ask your doctor if the scan is truly necessary. If yes, make sure you’re well-hydrated for 24 hours before and after. Tell your radiology team you have kidney disease. They may delay the scan or use a lower-dose contrast agent. In some cases, they’ll give you IV fluids before and after. Never skip this conversation-contrast dye can cause acute kidney injury in people with CKD.
Are there any supplements I should avoid with kidney disease?
Yes. Avoid supplements containing aristolochic acid, creatine, high-dose vitamin C, or herbal products like licorice root, green tea extract, or weight-loss teas. Many are unregulated and can cause kidney damage. Even some "kidney support" supplements contain hidden NSAIDs or heavy metals. Always check with your nephrologist before taking any supplement.
How often should I have my medications reviewed if I have CKD?
At least every 3 months if you have stage 3 or worse CKD. More often if your eGFR changes quickly, you’re hospitalized, or you start a new medication. A nephrologist or clinical pharmacist should review your full list-including over-the-counter drugs and supplements. Many patients get missed because they see multiple doctors. A single medication review can catch a dangerous interaction before it causes harm.
Final Thought: Your Kidneys Can’t Tell You When Something’s Wrong
Kidneys don’t scream. They whisper. By the time you feel tired, swollen, or off, the damage might already be done. Medication safety in kidney disease isn’t about avoiding all drugs. It’s about using the right ones, at the right dose, at the right time.That’s why knowledge is power. And why asking questions isn’t being difficult-it’s being smart. If you have CKD, your next doctor’s visit should start with this question: "What medications am I on that need a dose change based on my eGFR?"
Don’t wait for a crisis. Start today.





13 Comments