Learn how to safely take medications with kidney disease. Avoid nephrotoxins, understand eGFR-based dosing, and discover which drugs are safe-or dangerous-for chronic kidney disease.
Nephrotoxic Drugs: What They Are, Which Ones to Watch, and How to Stay Safe
When you take a medication, you expect it to help—not hurt your kidneys. But some common drugs, known as nephrotoxic drugs, medications that can cause direct damage to kidney tissue or impair kidney function. Also known as nephrotoxins, these substances don’t always show immediate signs, making them easy to overlook until kidney damage is already underway. The kidneys filter blood and remove waste, so when a drug interferes with that process, the effects can be serious—and sometimes permanent.
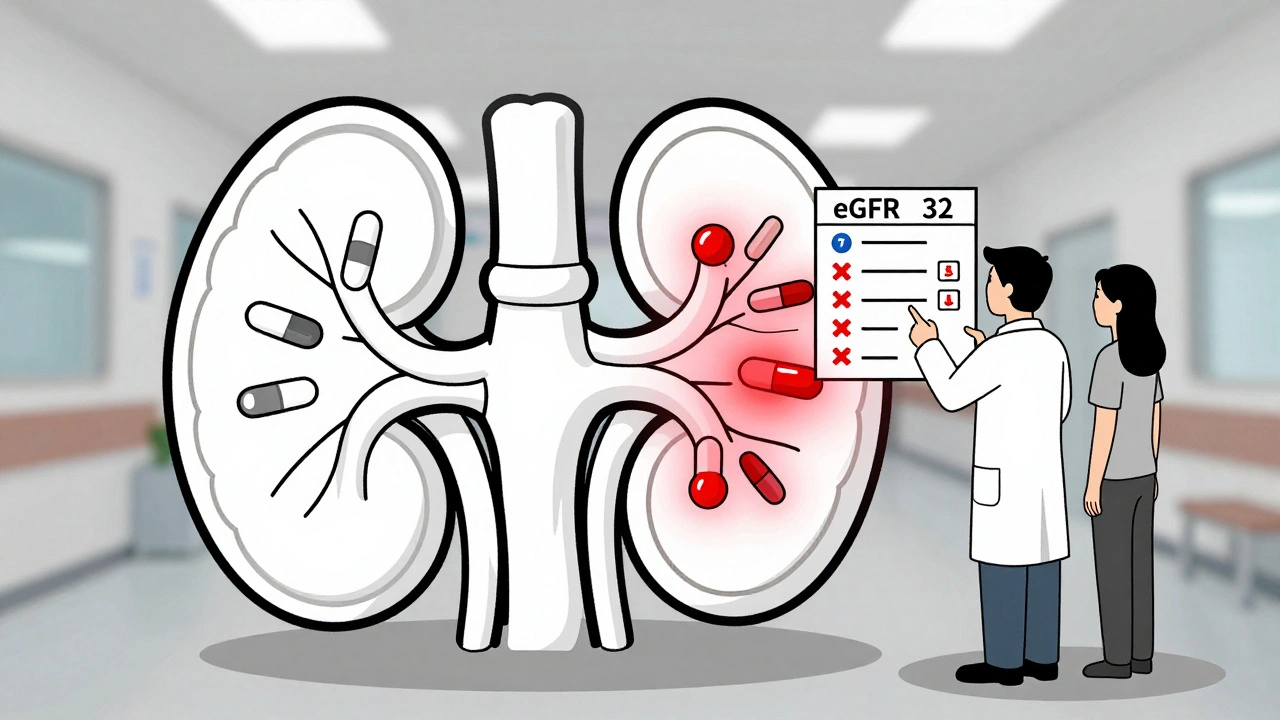
Nephrotoxic drugs aren’t rare. They include painkillers like ibuprofen and naproxen, antibiotics such as gentamicin and vancomycin, contrast dyes used in imaging scans, and even some blood pressure meds when used incorrectly. What makes them tricky is that they often work fine for most people—but if you’re older, have diabetes, or already have reduced kidney function, your risk jumps. That’s why medication dosing, the process of adjusting drug amounts based on individual factors like age, weight, and kidney health. Also known as renal dosing adjustments, it’s not just a suggestion—it’s a safety requirement. A standard dose for a healthy person might be toxic to someone with stage 3 kidney disease. That’s why kidney function, a measure of how well your kidneys filter waste, often tracked using eGFR or creatinine levels. Also known as renal function, it should be checked before starting long-term treatments.
Many people don’t realize that over-the-counter pain relievers can be just as risky as prescription drugs when taken daily. A study in the Journal of the American Society of Nephrology found that long-term NSAID users had a 20% higher chance of developing chronic kidney disease. Meanwhile, antibiotics like aminoglycosides can cause acute kidney injury in just a few days if not monitored. Even supplements like high-dose vitamin C or certain herbal remedies can add up, especially when combined with other meds. That’s why understanding drug interactions, how two or more medications affect each other’s behavior in the body. Also known as medication interactions, they matters as much as knowing the drug name itself.
You don’t need to avoid all these drugs—just use them wisely. If you’re on multiple medications, ask your doctor or pharmacist to review them for kidney risks. Get your kidney function tested annually if you’re over 60 or have high blood pressure or diabetes. Never ignore swelling, fatigue, or changes in urination—they could be early signs your kidneys are under stress. And if you’re traveling or managing a chronic condition, remember: what works for one person might not be safe for you.
Below, you’ll find real, practical guides from people who’ve been there—how to adjust doses safely, spot hidden risks in common meds, and protect your kidneys without giving up the treatments you need. No fluff. Just clear, actionable info to help you stay healthy while staying on your meds.