Why your generic medication might cost more than the brand name - it's not about quality, it's about insurance deals. Learn how tiered copays work and what you can do to save money.
Prescription Drug Tiers: How Your Insurance Decides What You Pay
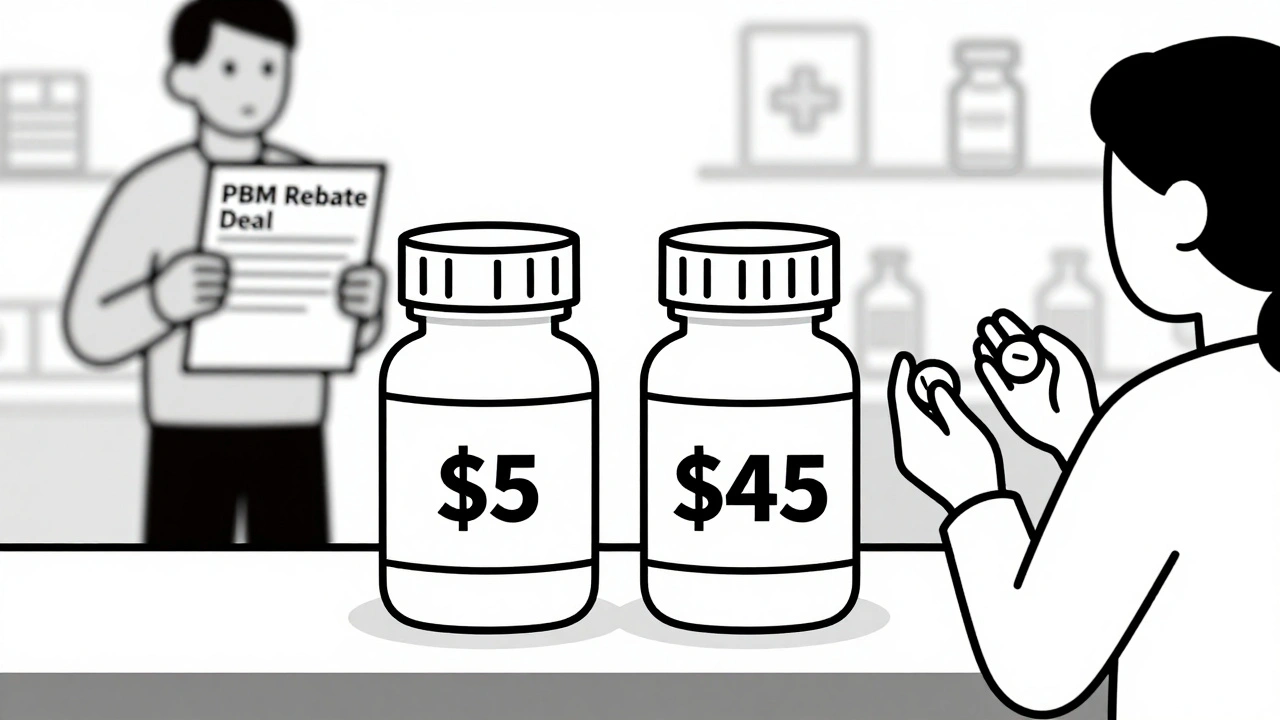
When you pick up a prescription, the price you pay isn’t just set by the drug company—it’s decided by your prescription drug tiers, a system insurers use to group medications by cost and coverage. Also known as formulary tiers, this structure determines whether you pay $5, $50, or $200 for the same medicine, depending on which bucket your drug falls into. It’s not about which drug is better—it’s about which one makes the most money for your insurer.
Pharmacy benefit managers, companies hired by insurers to manage drug lists and negotiate prices are the hidden force behind these tiers. They push for cheaper generics, demand rebates from big pharma, and often block brand-name drugs unless your doctor jumps through hoops. That’s why you might get a letter saying your usual pill is no longer covered—or why your $10 generic suddenly costs $40 because your plan moved it to a higher tier. And if you’re on a chronic condition like diabetes or high blood pressure, a single tier shift can add hundreds to your yearly bill.
These tiers aren’t random. They’re built around cost, not clinical need. Tier 1 usually has low-cost generics like metformin or lisinopril. Tier 2 might include slightly pricier brand-name drugs with generic alternatives. Tier 3 and 4? That’s where specialty meds live—drugs like biologics for arthritis or cancer treatments that cost thousands. And if your drug lands in Tier 5? You’re looking at prior authorization, step therapy, and maybe even a denial. The system doesn’t care if your body reacts badly to the cheaper option. It only cares about what’s cheapest for them.
That’s why so many of the articles below focus on the real-world fallout: people struggling with generic drug substitution, when insurers force you to switch to a cheaper version, even if it doesn’t work the same, or how insurer requirements, like prior authorizations and step therapy delay care and push patients to quit their meds. Some people skip doses. Others pay out of pocket. A few even stop treatment entirely because the cost became impossible.
What you’ll find here aren’t just explanations—they’re survival guides. From how to fight a tier change to spotting dangerous drug interactions when switching meds, these posts give you the tools to navigate a system stacked against you. You’ll learn how to read your formulary, what to say when your pharmacy says "it’s not covered," and how to find low-cost alternatives without risking your health. This isn’t theory. It’s what people are dealing with every day—just like you.