Learn how to safely take medications with kidney disease. Avoid nephrotoxins, understand eGFR-based dosing, and discover which drugs are safe-or dangerous-for chronic kidney disease.
Renal Dosing: How Kidney Function Changes Your Medication Needs
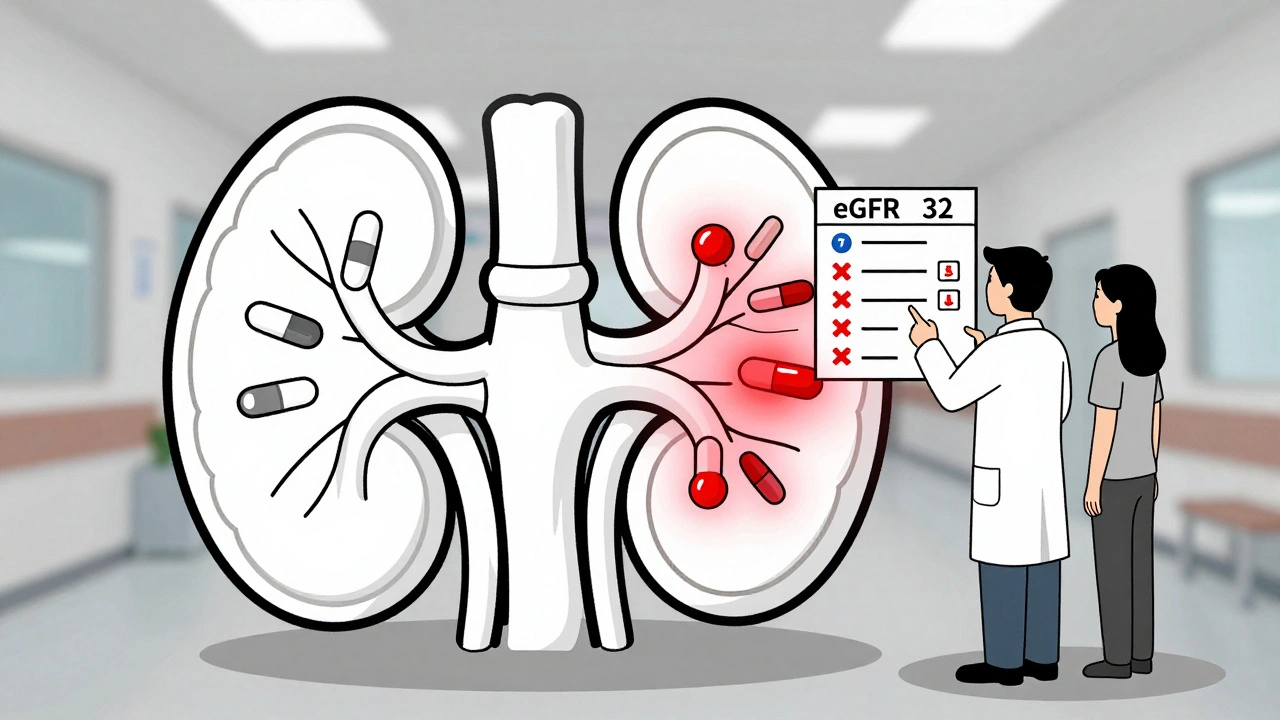
When your kidneys aren't working like they should, the way your body handles medication changes—renal dosing, the practice of adjusting drug amounts based on how well your kidneys filter waste. Also known as kidney-adjusted dosing, it's not just a medical detail—it's a safety rule that can keep you out of the hospital. Many common drugs, from painkillers to blood pressure pills, are cleared by your kidneys. If those filters are slow, the drug sticks around too long, turning a helpful dose into a dangerous one.
kidney function, how well your kidneys remove toxins and balance fluids is measured by tests like eGFR. A number below 60 often means you need lower doses. For example, someone with severe kidney disease might need half the normal dose of metformin or a completely different antibiotic than someone with healthy kidneys. medication dosing, the science of giving the right amount of a drug for the right person isn’t one-size-fits-all. Age, weight, and other drugs you take all play a role, but your kidneys are often the biggest factor.
Some medications, like certain antibiotics or seizure drugs, are especially risky if kidney function drops. Others, like insulin or some blood thinners, need less adjustment but still require attention. Even over-the-counter pain meds like ibuprofen can build up and damage your kidneys further if you're not careful. That’s why kidney disease, a condition where kidney function declines over time, often due to diabetes or high blood pressure isn’t just about fluid or diet—it’s about every pill you swallow.
Doctors don’t guess at renal dosing. They use formulas, lab results, and guidelines like KDIGO to make smart calls. But you can help by knowing your eGFR number, telling every provider about your kidney health, and asking: "Does this medicine need a dose change because of my kidneys?" Too many people take the same pills they always did—even after their kidneys slow down—and end up with confusion, falls, or worse.
What follows is a collection of real, practical posts that break down exactly how this works. You’ll find how anemia in kidney disease ties into treatment, how common drugs like theophylline or lisinopril need adjustments, and why supplement labels rarely warn you about kidney risks. You’ll also see how medication adherence becomes even more critical when your body processes drugs differently. This isn’t theory—it’s what happens in real lives, every day.