Renal Dosing Adjustments: What You Need to Know About Kidney Function and Medications
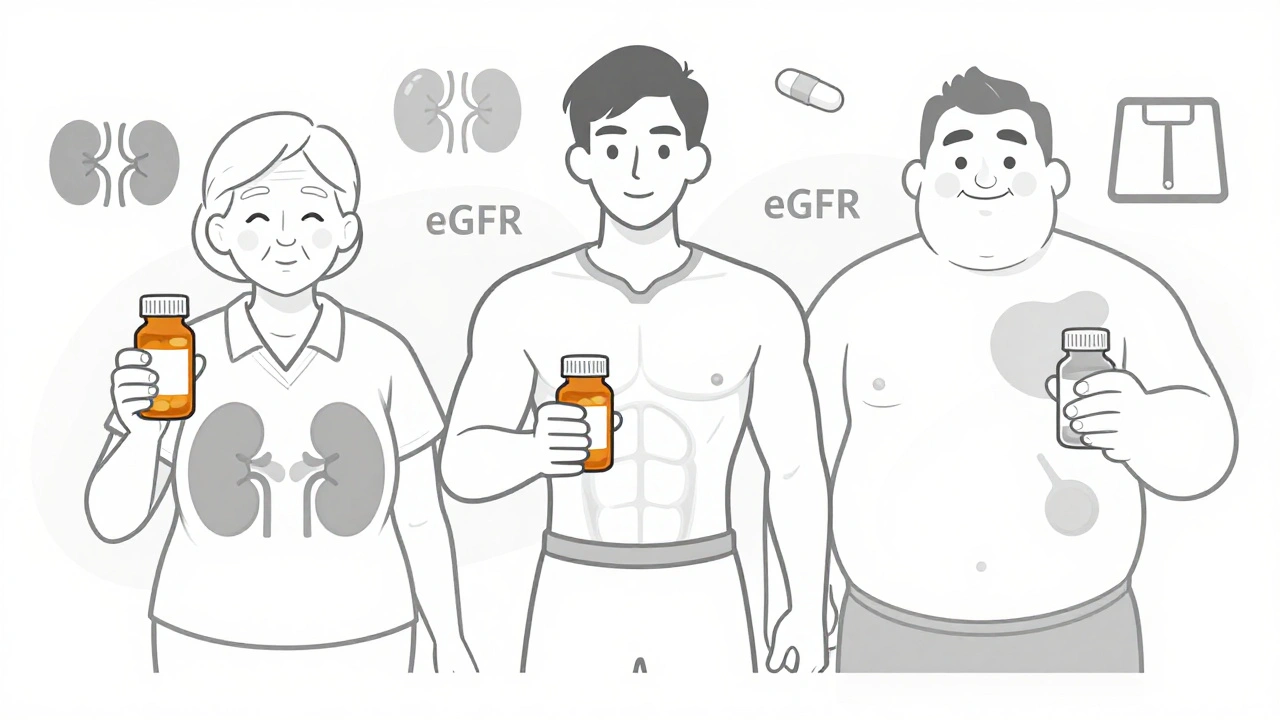
When your kidneys aren't filtering blood the way they should, many medications can build up to dangerous levels. This is where renal dosing adjustments, changes made to medication doses based on how well the kidneys are working. Also known as kidney-adjusted dosing, it's not optional for people with chronic kidney disease, older adults, or those on drugs cleared by the kidneys. If you're taking blood pressure pills, antibiotics, diabetes meds, or pain relievers, your kidney function could be changing how those drugs work in your body — without you even noticing.
Doctors check kidney function using simple tests like creatinine clearance, a measure of how fast your kidneys remove creatinine from your blood or estimated GFR. These numbers tell them if your kidneys are working at 30%, 50%, or 90% of normal. For drugs like metformin, vancomycin, or lisinopril-HCTZ, even a small drop in kidney function means the dose needs to go down — or the frequency needs to change. Too much of these drugs in your system can cause dizziness, low blood sugar, kidney damage, or even seizures. It’s not about being weak or old — it’s about chemistry. Your kidneys are your body’s main drug filter. When that filter gets clogged, the drugs don’t wash out like they should.
Some medications are safer than others when kidneys are impaired. But many common ones — like certain antibiotics, seizure drugs, or heart medications — have narrow safety margins. That means the difference between the right dose and a toxic one is small. That’s why drug clearance, how quickly the body removes a drug, often through the kidneys matters more than the pill you swallow. A 75-year-old on a standard dose of a diuretic might end up with dangerously low sodium. A diabetic on metformin with mild kidney disease might develop lactic acidosis. These aren’t rare mistakes — they’re predictable outcomes if kidney function isn’t checked.
You won’t always feel when your kidneys are slowing down. No pain. No warning. That’s why routine blood work is critical, especially if you’re on long-term meds. Many people think if they feel fine, their dose is fine. But that’s not true. The body can compensate for a while — until it can’t. And then the side effects hit fast.
In the posts below, you’ll find real-world examples of how renal dosing adjustments affect everyday medications. From how lisinopril-HCTZ can cause dizziness when kidney function drops, to why theophylline becomes toxic in people with kidney disease, to how diabetes meds need to be tweaked when creatinine clearance falls below 60 mL/min. These aren’t theory pages. They’re practical guides from people who’ve been there — patients and providers alike. You’ll learn what to ask your doctor, what lab numbers to track, and which meds are safest when your kidneys aren’t at 100%.