Discover the best app-based prescribing platforms for affordable generic medications in 2025. Compare Amazon RxPass, Ro, Hims & Hers, and Beem Health to save up to 85% on everyday prescriptions.
Telehealth Prescriptions: How Online Doctor Visits Are Changing How You Get Medication
When you need a prescription, you don’t always have to sit in a waiting room anymore. Telehealth prescriptions, a way to get medication after a video or phone visit with a licensed provider. Also known as virtual care prescriptions, they’re now a normal part of how people manage everything from high blood pressure to antibiotics. This isn’t just convenience—it’s access. For people in rural areas, those with mobility issues, or anyone juggling work and family, getting a prescription without driving across town changes everything.
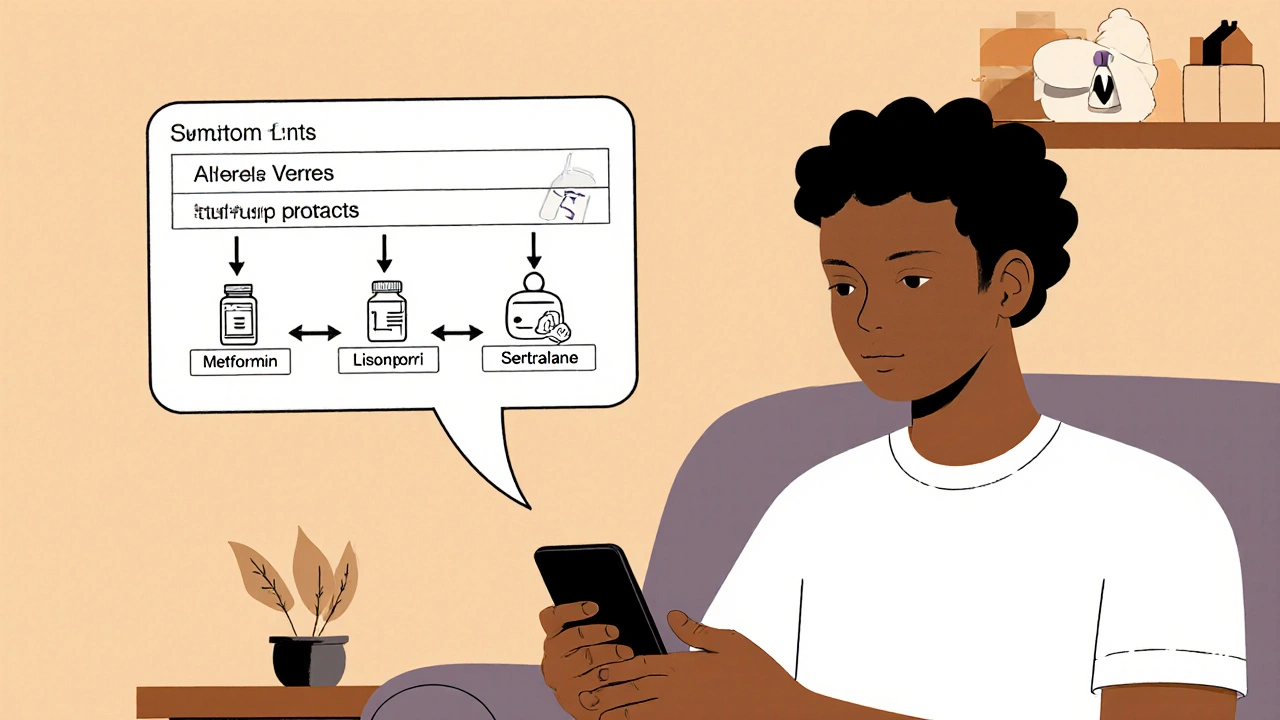
Telehealth prescriptions aren’t magic. They still require a real medical evaluation. A doctor or nurse practitioner reviews your symptoms, checks your history, and decides if a prescription is safe and needed. You can’t just ask for a refill on a chat app and get it instantly. But you can talk to a provider while sitting on your couch, describe your sore throat, and have the script sent to your local pharmacy—all in under 30 minutes. It works for common issues like sinus infections, UTIs, allergies, and even mental health meds like antidepressants. Some states even allow prescriptions for chronic conditions like diabetes or thyroid problems through telehealth, as long as you’ve had an in-person visit within the last year.
Behind the scenes, this system relies on digital health, the use of technology to deliver medical care and manage health data. Electronic health records, secure messaging platforms, and e-prescribing systems all connect to make sure your info is safe and your meds are accurate. It’s not just about video calls—it’s about integrated systems that keep your care coordinated. That’s why some pharmacies now flag telehealth scripts for extra review, especially for controlled substances. They’re not being suspicious—they’re being careful.
Not every condition qualifies. You won’t get a prescription for a broken bone or a rash that needs a physical exam through telehealth alone. But for the majority of routine, repeatable, or manageable conditions, it’s faster, cheaper, and just as effective. Studies show patients are just as satisfied with telehealth prescriptions as they are with in-person visits. And for people who’ve struggled to get care because of cost, time, or transportation, it’s often the only option that works.
There’s also the question of remote prescribing, the legal and practical process of issuing medication orders without a face-to-face exam. Rules vary by state and by drug type. Some states require a video call; others allow phone-only visits for refills. Controlled substances like Adderall or oxycodone have extra restrictions. But for most antibiotics, blood pressure meds, or birth control, the process is smooth—if you’re using a legitimate provider. Watch out for websites that promise instant prescriptions without any questions. Those aren’t telehealth—they’re scams.
What you’ll find in the posts below are real stories and facts about how telehealth prescriptions fit into everyday health care. You’ll see how people use them for common issues, what pitfalls to avoid, how insurance covers them, and how they connect with other trends like medication shortages and patient education. Whether you’re considering your first virtual visit or just wondering if it’s safe, these articles give you the straight facts—no fluff, no hype, just what you need to know to make smart choices.