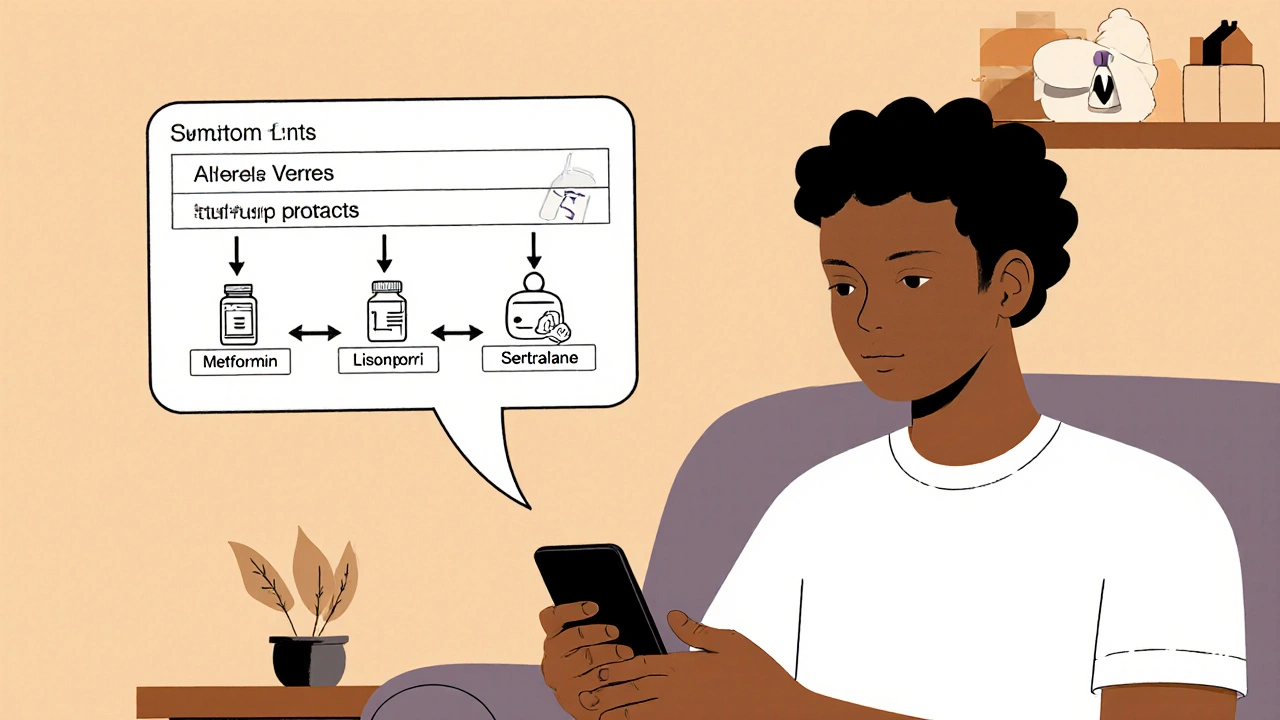
Getting generic medications used to mean driving to the pharmacy, waiting in line, and paying full price - even when the drug was identical to the brand-name version. Today, you can do it all from your phone in under 20 minutes. App-based prescribing platforms have changed how millions of people access everyday meds like metformin, lisinopril, and sertraline. No more awkward conversations with the pharmacist. No more $80 co-pays for pills that cost $5 to make. Just tap, answer a few questions, and get your generics delivered to your door - often the same day.
How App-Based Prescribing Actually Works
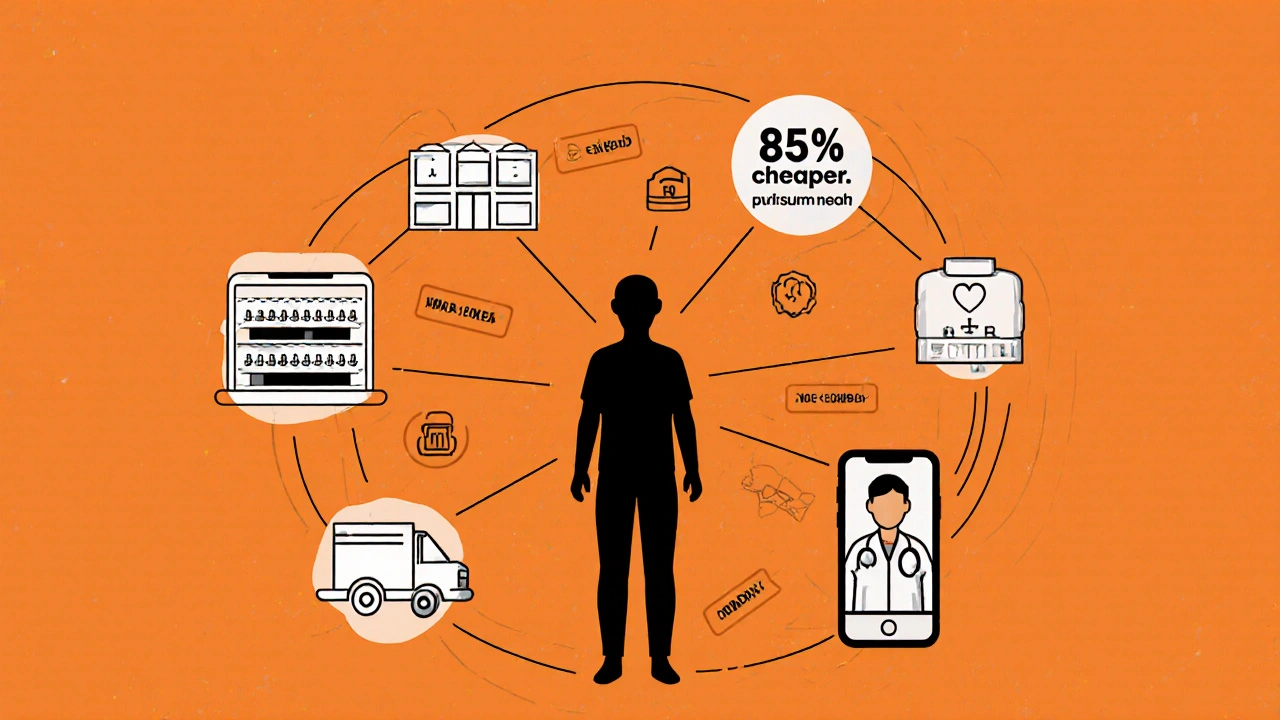
It’s not magic. It’s a simple pipeline: you answer medical questions in an app, a licensed doctor reviews your info, and if it’s safe, they send an e-prescription to a partnered pharmacy. The pharmacy fills it, ships it, and you get a text when it’s on the way. The whole process takes 12 to 18 minutes on average - compared to 24 to 72 hours with a traditional doctor’s visit.
These apps don’t just guess what you need. They use AI to match your symptoms with approved generic medications. If you report high blood pressure, the system checks your age, weight, allergies, and current meds before suggesting a generic ACE inhibitor like lisinopril. It won’t prescribe opioids, stimulants, or anything controlled. That’s by design - safety filters block risky prescriptions.
Most apps require iOS 14 or Android 9.0 and are under 85MB. They use end-to-end 256-bit AES encryption, biometric login (Face ID or fingerprint), and are fully HIPAA-compliant. Your data doesn’t leave the secure cloud. You’re not just saving money - you’re getting enterprise-grade privacy.
Top Platforms for Generic Medications in 2025
Not all apps are built the same. Here’s who’s leading the pack and what they actually offer.
Amazon RxPass
Launched in September 2023, Amazon RxPass is the cheapest option if you’re a Prime member. Pay $5 a month, and you get unlimited access to over 150 generic medications - no per-pill fees. That includes common drugs like atorvastatin, levothyroxine, and omeprazole. If you take three or more generics monthly, this pays for itself in one visit.
But here’s the catch: only 150 meds are covered. If you need something outside that list - say, a less common thyroid med or a specific antidepressant - you’re out of luck. Amazon doesn’t offer doctor consultations. You pick from their pre-approved list. It’s simple, but limited. Users report 3.5/5 on Trustpilot, mostly because of the narrow selection.
Ro
Ro is the most comprehensive. With over 1,200 generic medications across 15 conditions - from acne to anxiety to diabetes - it’s the closest thing to a full-service digital clinic. You get video consults with board-certified doctors in all 50 states. Their prescription approval rate is around 70%, higher than most competitors because they take time to review your history.
Ro charges $15/month plus medication costs. That’s more than Amazon, but you get more. They’ve integrated with Apple Health so your prescription history syncs with your other health data. Their diabetes program saw 89% adherence rates - way above the 67% average in traditional care. If you’re managing a chronic condition, Ro is the most reliable.
Hims & Hers
Hims & Hers owns the lifestyle meds space. If you need finasteride for hair loss, sildenafil for ED, or tretinoin for acne, this is your go-to. They don’t try to be everything. They focus on 4-5 high-demand categories and do it well. Their generics are priced 40-60% below retail pharmacy rates.
They don’t offer the broadest list - only about 300 meds - but they’re experts in what they cover. Their branding is clean, discreet, and user-friendly. Reviews are solid at 3.9/5. But if you have multiple health issues or complex meds, you’ll need another platform. It’s not built for full-spectrum care.
Beem Health
Beem Health is the wildcard. It’s not just a pharmacy app - it’s a financial health tool. You get access to over 900 generics, but also cash advances up to $1,000 through their Everdraft™ feature. If your prescription costs $45 and you’re short on cash, you can get the money upfront and pay it back over time.
They serve 5.1 million users as of August 2025 and have the highest Trustpilot score at 4.2/5. People love that they don’t have to choose between paying rent and filling a prescription. Their integration with pharmacy networks is strong, and they offer pharmacist chat support. The downside? Their app feels more like a fintech platform than a health tool - which works for some, but confuses others.
How Much Do You Really Save?
Let’s say you take metformin 500mg twice daily. At your local pharmacy, it costs $45 a month with insurance. Without insurance? $120.
On Amazon RxPass? $0 extra - it’s covered in your $5/month fee.
On Ro? $12 for the med, plus $15/month subscription. Total: $27.
On Hims & Hers? $28 for the med, one-time $30 consultation fee. Total: $58 - but if you only need it once, that’s fine.
Beem Health? $15 for the med, no subscription. You pay only for what you use. If you’re on a tight budget, that’s ideal.
According to Beem Health’s July 2025 analysis, users save 30-50% on average compared to retail pharmacies. Drug Patent Watch’s 2025 report says generics on these platforms cost 80-85% less than brand names. That’s not marketing - that’s the real cost difference.
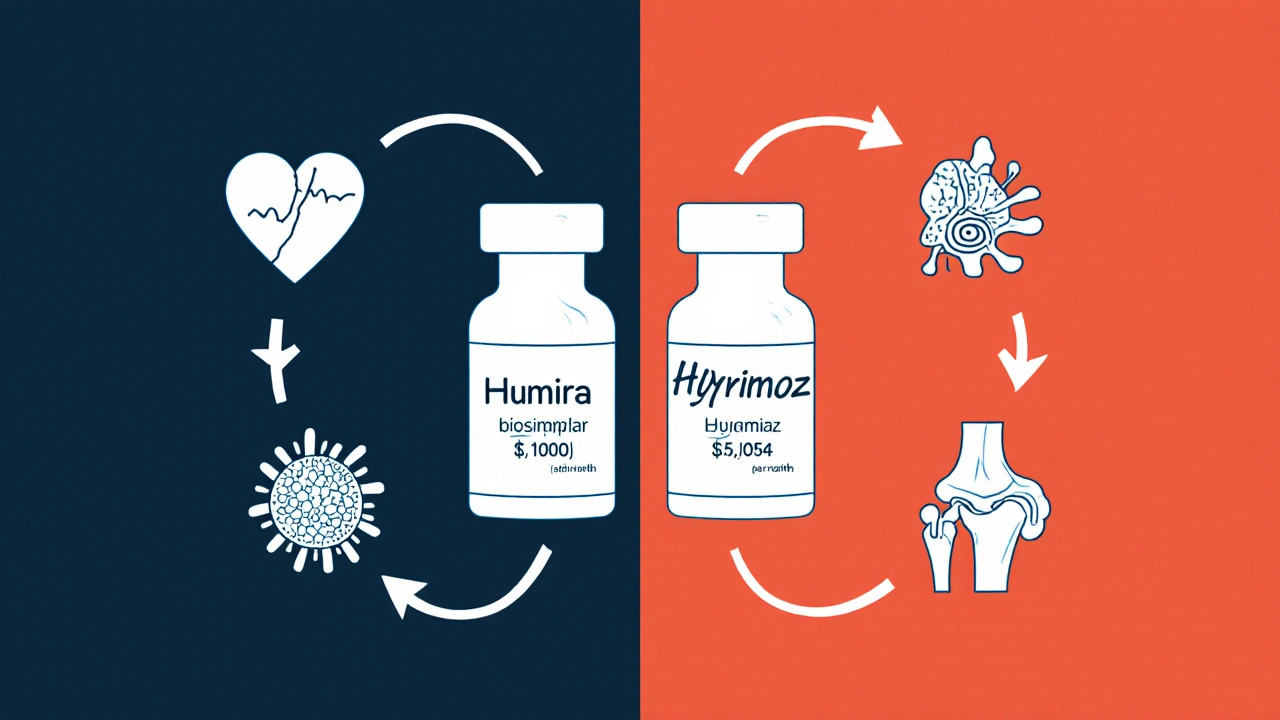
What’s Not Covered - And Why
These apps won’t prescribe controlled substances. No Adderall. No oxycodone. No benzodiazepines. That’s not a glitch - it’s federal law. Even if you’ve been on it for years, you still need an in-person visit for refills.
Also, they won’t handle complex cases. If you’re on five meds, have kidney disease, or are pregnant, you’ll likely get denied. The AI and doctors play it safe. That’s a feature, not a bug - but it can be frustrating if you’re used to getting everything online.
State laws matter too. In 22 states, you need an established relationship with a provider before getting a prescription. That means if you just moved, you might be blocked until you’ve seen a local doctor. It’s not the app’s fault - it’s regulation.
Real User Problems - And How to Fix Them
Most people love the convenience. But complaints are real.
- Prescription denied - Happens in 25-35% of first attempts. Don’t panic. The system flagged something. Upload your past prescriptions or medical records. Often, a second review approves it.
- Insurance doesn’t work - 40% of users try to use insurance and get stuck. These apps rarely integrate with insurance. Pay out-of-pocket. It’s still cheaper.
- Delivery delays - 18% report late shipments. Check if your zip code is in the delivery zone. Some rural areas take 3-5 days.
- Medication substitution - You ordered levothyroxine 88mcg. You got 75mcg. This happens when pharmacies switch brands. Call the pharmacy. Ask for the exact generic you were prescribed. They’re required to honor it.
- No human support - Amazon’s chat is fast but robotic. Ro’s pharmacist line takes 47 minutes. If you need help, call the pharmacy directly. They often have better answers.
Reddit’s r/telehealth has over 45,000 members. Search for your drug + “app denied.” You’ll find solutions. One top tip: always upload clear photos of past prescriptions. OCR tech reads them better when they’re sharp and well-lit.
Who Should Use These Apps - And Who Shouldn’t
Use them if:
- You take 1-3 common generics monthly
- You’re between 25 and 44 years old (52% of users are in this group)
- You want privacy for sensitive conditions (ED, anxiety, acne)
- You don’t have easy access to a primary care doctor
Don’t use them if:
- You’re on complex meds (5+ drugs, chronic kidney/liver disease)
- You’re over 65 and on Medicare - most apps don’t integrate with Part D yet (Beem Health is working on it for 2026)
- You need frequent lab tests or dosage adjustments
- You’re uncomfortable with digital-only care
For seniors or those with multiple conditions, stick with your local pharmacist and doctor. These apps are great for routine meds - not for managing complex health.
The Bigger Picture: Risks and the Future
There’s real concern in the medical community. A 2025 JAMA study found telehealth platforms prescribe medications 23% more often than traditional clinics for the same symptoms. That’s not always because patients need more drugs - sometimes it’s because the model is designed to convert consultations into sales.
The FDA issued 12 warning letters in early 2025 to companies for downplaying side effects. The American Medical Association warns of “therapeutic misconception” - when people think a quick app visit equals real care.
But the demand isn’t going away. 38% of Americans have used one of these apps by 2025. Employers are adding them to health plans. Apple and Google are integrating them into their health ecosystems. Ro is syncing with Apple Health. Beem is building Medicare links.
The future? Hybrid care. Apps for routine meds. In-person visits for complex issues. Real-time data sharing between pharmacies and digital platforms to avoid dangerous interactions. Pilot programs are already live in 12 states.
For now, these apps are a powerful tool - if you use them right. They’re not a replacement for your doctor. But for everyday generics? They’re faster, cheaper, and more private than anything we’ve had before.
Are app-based prescriptions legal?
Yes. All licensed platforms use U.S.-based, board-certified physicians who follow state and federal telehealth laws. Prescriptions are sent electronically to partnered pharmacies that are fully licensed. The FDA regulates the drugs themselves - not the delivery method - as long as the prescribing doctor is properly credentialed.
Can I use insurance with these apps?
Most don’t accept insurance directly. They operate as cash-pay services, which is why prices are so low - they avoid insurance billing overhead. You pay out-of-pocket, but you’re still saving 30-85% compared to pharmacy retail prices. Some platforms, like Beem Health, are working on Medicare Part D integration for 2026.
What if my prescription gets denied?
Denials happen in 25-35% of cases, usually because of incomplete info, drug interactions, or state restrictions. Don’t give up. Upload past prescriptions, lab results, or medical records. Many platforms allow a second review. If it’s denied again, consult your primary care provider - they can still prescribe the same generic through traditional channels.
Are generic drugs from these apps safe?
Yes. All generics are FDA-approved and sourced from U.S.-licensed pharmacies. They contain the same active ingredients as brand-name drugs. The only difference is the inactive fillers - which don’t affect effectiveness. Many are made by the same manufacturers as brand-name versions. Look for the “ANDA” (Abbreviated New Drug Application) number on the packaging to confirm FDA approval.
How fast do I get my meds?
Most orders are filled within 24 hours. Same-day delivery is available in major cities for an extra fee. Standard shipping takes 2-5 business days. Delivery times depend on your location and the pharmacy’s processing speed. You’ll get real-time tracking in the app.
Can I switch between platforms?
You can, but don’t use multiple platforms at once. Each app keeps its own record. If you’re taking meds from Ro and Hims & Hers, your doctors and pharmacists won’t see the full picture - increasing the risk of dangerous interactions. Pick one primary platform for routine meds, and use your local pharmacy for anything complex.
Do these apps work outside the U.S.?
No. These platforms are only available in the U.S. due to licensing, pharmacy regulations, and shipping laws. If you’re outside the U.S., look for local digital health services - countries like Canada, the U.K., and Australia have their own regulated telehealth pharmacy systems.





8 Comments