Why your generic medication might cost more than the brand name - it's not about quality, it's about insurance deals. Learn how tiered copays work and what you can do to save money.
Tiered Copays: How Drug Costs Work and What It Means for Your Prescription Budget
When you pick up a prescription, the amount you pay isn’t set by the pharmacy—it’s decided by your tiered copays, a system where insurance plans divide medications into cost levels based on price and preference. Also known as formulary tiers, this structure tells you exactly how much you’ll fork out for each drug, and it’s not always what you expect. It’s not about the drug’s effectiveness. It’s about whether your insurer considers it a generic, preferred brand, or non-preferred specialty medication. That label determines your share of the cost.
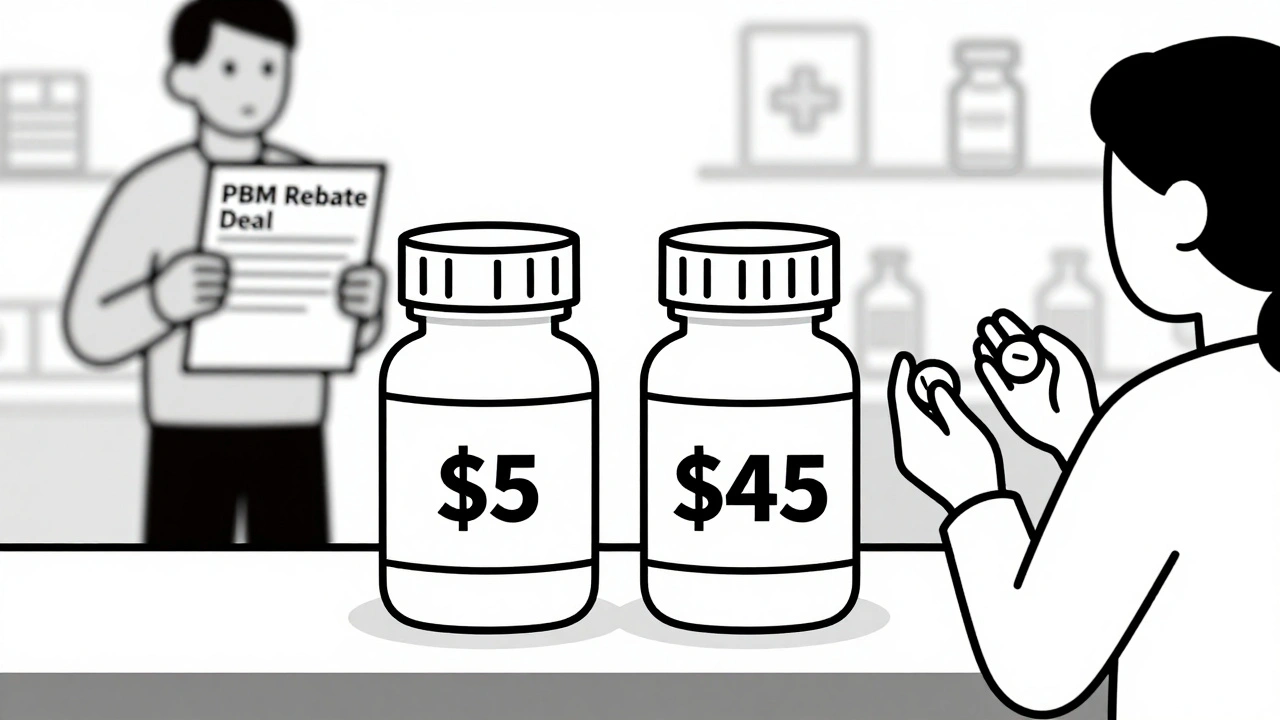
Most plans have three to five tiers. Tier 1 is usually generic drugs—low cost, high value. You might pay $5 or $10. Tier 2 is brand-name drugs that your insurer prefers because they’ve negotiated lower prices. Tier 3 is non-preferred brands, where you could pay $40 or more. Tier 4 and 5? Those are specialty drugs—like those for rheumatoid arthritis, hepatitis C, or cancer. These can cost hundreds, even over $1,000 per month. The kicker? Your insurer doesn’t always tell you which tier a drug is in until you’re at the counter. And if you’re on a high-tier drug, switching to a lower one could save you hundreds a month. That’s why knowing your plan’s formulary isn’t optional—it’s essential.
It’s not just about the drug itself. drug formularies, lists of covered medications organized by tier. Also known as preferred drug lists, they’re updated often, sometimes without notice. A drug you’ve been taking for years might suddenly move from Tier 2 to Tier 3 because the insurer struck a new deal with a competitor. Or your insurer might require you to try a cheaper generic first—this is called step therapy. If you skip that step, you pay full price. And if you’re on multiple meds, the math gets messy fast. One drug might be on Tier 1, another on Tier 4. You could be paying $15 for one and $350 for another, even if they treat the same condition.
People with chronic conditions—like diabetes, high blood pressure, or asthma—are hit hardest. Their meds are often long-term, and even small increases add up. A $20 increase on a monthly pill? That’s $240 a year. Multiply that by three or four drugs, and you’re talking about a rent payment. That’s why many turn to medication affordability, strategies to reduce out-of-pocket drug expenses through alternatives, coupons, or assistance programs. Some use mail-order pharmacies. Others ask their doctor for samples or switch to generics. Community clinics and apps now help people find cheaper options, sometimes cutting costs by 80%.
It’s not just about money—it’s about access. If you can’t afford your drug, you skip doses. You cut pills in half. You stop taking them. That’s when health problems get worse, ER visits go up, and hospital stays follow. Tiered copays weren’t designed to punish people. But without transparency, they often end up doing exactly that.
Below, you’ll find real-world guides on how to spot hidden costs, challenge insurance decisions, switch to lower-tier drugs safely, and even find free or low-cost alternatives when your copay feels impossible. These aren’t theoretical tips—they’re actions people have taken to cut their prescription bills in half. You don’t need to be an expert. You just need to know where to look.