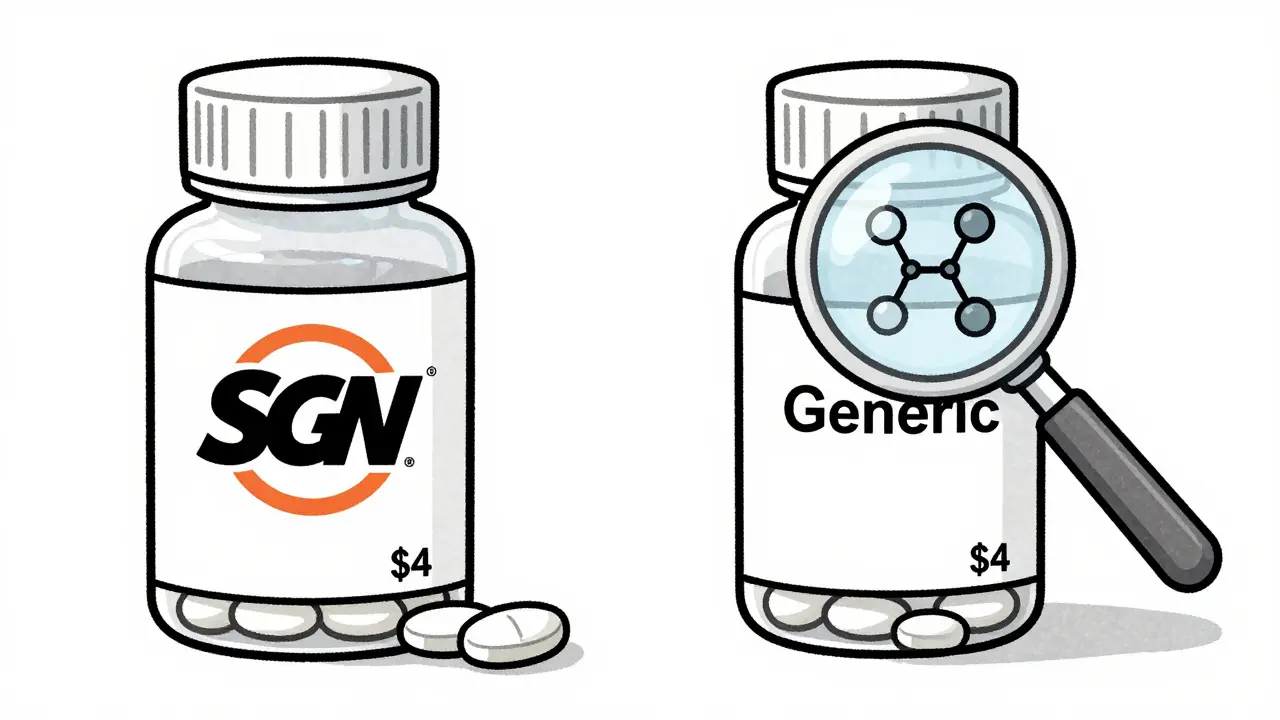
When you pick up a prescription, you might see two options: the brand-name drug you’ve heard of, and a much cheaper generic version. The price difference is staggering-sometimes generic drugs cost 80-85% less than the brand. But here’s the real question: if they’re so much cheaper, are they any good?
They’re the Same Medicine, Just Without the Branding
Generic drugs aren’t cheap knockoffs. They’re exact copies of brand-name drugs in every way that matters. The active ingredient-the part that actually treats your condition-is identical. So is the strength, the dosage form (pill, liquid, injection), and how it’s absorbed by your body. The U.S. Food and Drug Administration (FDA) requires generics to meet the same strict standards for safety, purity, and effectiveness as the original.Think of it like buying a smartphone. One version comes in a fancy box with a logo you recognize. The other is plain, no logo, same screen, same processor, same battery life. The only difference? Price. Generic drugs work the same way. They’re not cheaper because they’re lower quality. They’re cheaper because they don’t carry the weight of the original development costs.
Why Brand-Name Drugs Cost So Much
Developing a new drug isn’t just expensive-it’s a marathon that takes 8 to 12 years and costs an average of $2.6 billion. That money goes into years of lab research, animal testing, and multiple rounds of human clinical trials. Companies need to recover that investment before other manufacturers can copy the drug. That’s why brand-name drugs get 20 years of patent protection from the date they’re first filed. During that time, only the original company can sell it.That exclusivity lets them set high prices. A drug like Lipitor (atorvastatin) for cholesterol used to cost over $500 a month. Once the patent expired, the generic version dropped to around $4. That’s not because the generic is weaker-it’s because the company making it didn’t have to spend billions to prove the drug works.
How Generics Skip the Costly Steps
Generic manufacturers don’t need to repeat all the expensive testing. Thanks to the Hatch-Waxman Act of 1984, they only need to prove their version is bioequivalent to the brand. That means the generic delivers the same amount of active ingredient into your bloodstream at the same rate as the brand-name drug. The FDA requires this difference to be within 80-125%-a tight range that ensures no meaningful difference in how the drug works.That shortcut cuts development time from over a decade to just 1-3 years. And instead of spending billions, generic companies spend between $1 million and $5 million per drug to get approval. That’s a massive difference. The FDA doesn’t require them to repeat animal or human clinical trials. They focus instead on making sure the manufacturing process meets the same quality standards-called Current Good Manufacturing Practices (CGMP)-as the brand-name maker.
Same Rules, Different Price Tag
You might wonder: if generics are cheaper, do they cut corners on quality? They don’t. The FDA inspects over 12,000 drug manufacturing sites worldwide every year. These inspections cover both brand-name and generic factories. A generic pill made in India or the U.S. must meet the same standards as the brand. The color, shape, or flavor might be different-that’s just because trademark laws prevent generics from looking exactly like the brand. But the active ingredient? Identical.Stability testing is also the same. Both types of drugs must prove they stay effective and safe for their full shelf life-usually 12 to 24 months of testing. The FDA requires generics to stay within 90-110% of their labeled potency. That’s not a loophole. That’s the same standard used for brand-name drugs.
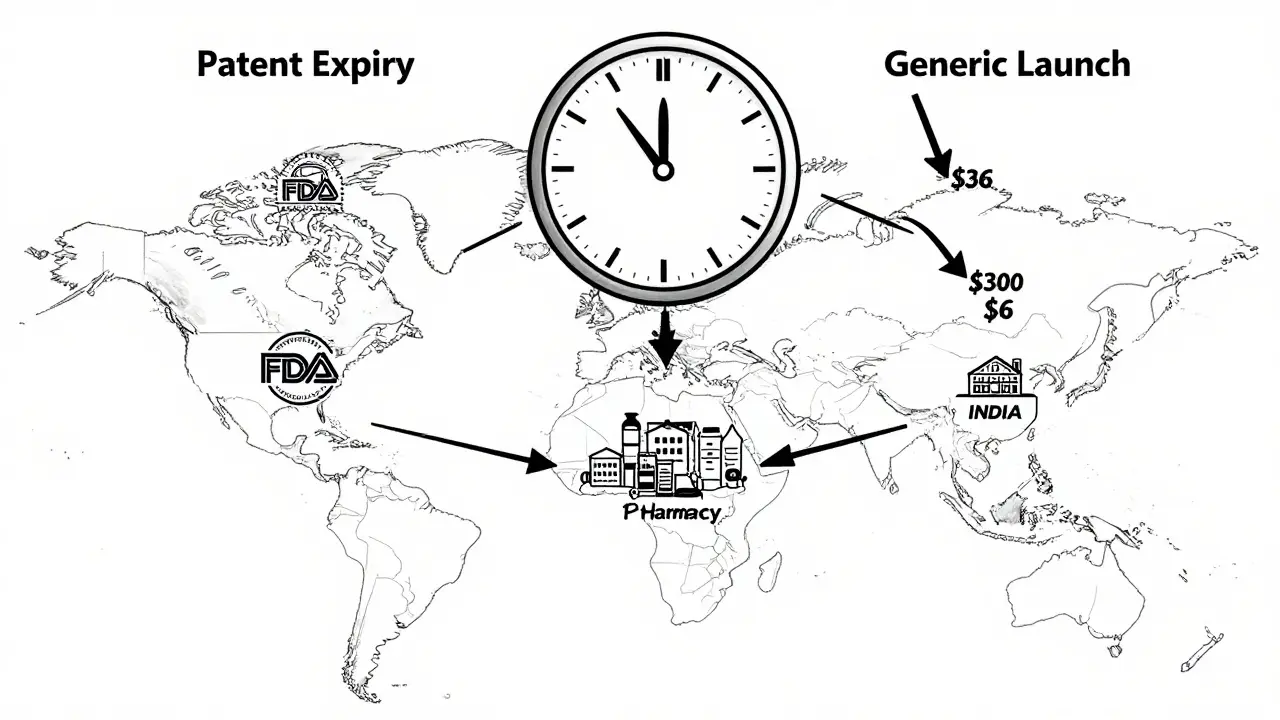
Competition Drives Prices Down
Once a patent expires, multiple companies can start making the generic. The more manufacturers enter the market, the lower prices go. On average, 14 different companies make the same generic drug. In some cases, there are over 50. That kind of competition forces prices to plummet. The Congressional Budget Office found that within the first year after a generic enters the market, prices drop by 80-90%. By the time five or more companies are selling it, the price often falls to just a few dollars per month.Take omeprazole, the generic for Prilosec. When it was brand-only, it cost $300 a month. Now, you can buy it for $6. Same drug. Same effect. Same safety profile. The only thing that changed? The number of companies making it.
Generics Are Used Everywhere-Because They Work
In the U.S., generics make up 90.5% of all prescriptions filled. But they account for only 18% of total drug spending. That means for every dollar spent on prescriptions, 82 cents goes to brand-name drugs-even though they’re prescribed far less often. In 2022 alone, generic drugs saved the U.S. healthcare system $293 billion. That’s not a guess. That’s a number from the Association for Accessible Medicines.People are catching on. A 2023 survey by Tebra found that 63% of Americans choose generics over brand-name drugs. Most do it because of cost. But even among those who still prefer brands, 84% admit generics are just as effective. The problem isn’t performance-it’s perception.
Why Some People Still Doubt Generics
Despite the evidence, skepticism lingers. Some patients report feeling different after switching from brand to generic. In rare cases, especially with drugs that have a narrow therapeutic index-like warfarin (blood thinner) or levothyroxine (thyroid hormone)-even tiny changes in blood levels can matter. That’s why some doctors prefer to keep patients on the same version, whether brand or generic.But here’s the key: the FDA says all approved generics are interchangeable. If a patient feels worse after switching, it’s rarely because the generic is inferior. More often, it’s because they’re now taking a different manufacturer’s version. Even two generics made by different companies can have slightly different inactive ingredients (fillers, dyes, coatings), which might affect how quickly the pill dissolves in the stomach. For most people, that doesn’t matter. For a small group, it might.
That’s why pharmacists are trained to talk to patients when switching. They’re supposed to explain that the active ingredient hasn’t changed, even if the pill looks different. The American Pharmacists Association recommends spending 3-5 minutes with each patient on a new generic prescription.
Insurance Makes Generics Even Cheaper
Most insurance plans encourage generics by putting them in the lowest cost tier. You might pay $0-$15 for a generic, but $25-$50 for a brand-name drug-even if it’s the same medicine. Some plans won’t cover the brand at all unless your doctor proves you need it. If you ask for the brand when a generic is available, your insurer might deny coverage unless your doctor files a special request.That’s not a trick. It’s how the system is built to save money-for you, your insurer, and the whole healthcare system. In 2023, RxOutreach reported a 28% increase in patients signing up for assistance programs because they couldn’t afford brand-name drugs. The average monthly savings? $317 per medication.
What’s Next for Generic Drugs?
The FDA is working to speed up approval for complex generics-like inhalers, injectables, and topical creams-that used to take years to get approved. Their new 2023 guidance aims to cut approval times from five years to two. That could save consumers another $50 billion a year.Meanwhile, the government is cracking down on "pay-for-delay" deals, where brand-name companies pay generic makers to hold off on releasing their cheaper versions. The FTC found 148 such deals in 2022, costing consumers $3.5 billion annually. Those practices are being challenged in court.
And as more big drugs lose patent protection-150 are set to expire by 2028-generic savings will keep growing. The Congressional Budget Office predicts that by 2028, 93% of all prescriptions will be generics.
Bottom Line: Save Money Without Sacrificing Care
Generic drugs aren’t a compromise. They’re the smart choice. They’re the same medicine, made to the same standards, at a fraction of the cost. The only real difference? Your wallet.If your doctor prescribes a brand-name drug, ask: "Is there a generic?" If your pharmacist switches you to a generic, don’t panic. Check the pill, yes-but know this: the active ingredient hasn’t changed. And if you’re worried about side effects, talk to your provider. But don’t assume the generic is the problem. It’s usually not.
For millions of people, generics mean the difference between taking their medicine and skipping it because they can’t afford it. That’s not just economics. That’s healthcare.
Are generic drugs as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove they’re bioequivalent-meaning they deliver the same amount of medicine into your bloodstream at the same rate. Thousands of studies and decades of real-world use confirm that generics work just as well.
Why do generic pills look different from brand-name pills?
Trademark laws prevent generic manufacturers from making their pills look identical to the brand-name version. That’s why the color, shape, or size might be different. But those changes only affect appearance-not how the drug works. The active ingredient and how it’s absorbed remain the same.
Can I trust generics made in other countries?
Yes. The FDA inspects all manufacturing facilities worldwide-whether they’re in the U.S., India, China, or elsewhere. All factories must meet the same strict standards for cleanliness, quality control, and testing. Over 12,000 inspections are done each year. If a facility fails, the FDA blocks its products from entering the U.S. market.
Why do some people say generics don’t work for them?
For most people, this isn’t true. But for a small number taking drugs with a narrow therapeutic index-like warfarin or levothyroxine-switching between different generic manufacturers might cause slight variations in how the drug is absorbed. That’s why some doctors prefer to stick with one version. It’s not because generics are inferior-it’s about consistency for sensitive medications.
Do insurance plans push generics on purpose?
Yes. Most insurance plans have a tiered system where generics are the cheapest option. You’ll pay less out of pocket for a generic, and sometimes your plan won’t cover the brand-name version unless your doctor proves it’s medically necessary. This isn’t a trick-it’s how the system is designed to reduce overall drug costs.
Are there any risks in switching from brand to generic?
For 99% of medications, there’s no risk. The FDA approves generics only after proving they’re bioequivalent. But if you’re taking a drug with a narrow therapeutic index, your doctor might monitor you more closely after switching. Always talk to your pharmacist or provider before switching-especially if you’ve had issues before.
What to Do Next
If you’re paying full price for a brand-name drug, ask your doctor or pharmacist: "Is there a generic?" If you’re already taking a generic and have concerns, don’t assume it’s broken. Talk to your provider. Ask if the change in appearance or cost could be affecting your perception-not your health.Most importantly: don’t skip your meds because of cost. Generics exist to make treatment affordable. They’re not a second choice. They’re the standard.








14 Comments