When your immune system turns against your own body, things get messy. Instead of fighting off germs, it starts attacking your joints, skin, or gut. That’s what happens in autoimmune diseases like rheumatoid arthritis, psoriasis, or Crohn’s disease. For decades, doctors relied on drugs that dampened the whole immune system-like methotrexate or azathioprine. They helped, but often not enough. And they came with side effects that made people feel worse than the disease itself.
Then came TNF inhibitors. These weren’t just another pill. They were a revolution. Designed to target one specific troublemaker-tumor necrosis factor alpha (TNFα)-they stopped the inflammation at its source. For many people, it meant going from barely walking to hiking again. From constant pain to quiet mornings. But they’re not magic. And they’re not for everyone.
What Is TNF Alpha, and Why Does It Matter?
TNFα isn’t evil by nature. It’s a signaling protein your body makes naturally. When you get an infection, TNFα sounds the alarm. It tells immune cells to rush to the site, raises your temperature to fight germs, and helps seal off damaged tissue. It’s part of survival.
But in autoimmune diseases, this system goes haywire. TNFα keeps firing even when there’s no infection. It becomes a constant, low-grade alarm bell. That’s when your joints swell, your skin flakes, your intestines get inflamed. TNFα doesn’t just cause inflammation-it keeps it going. It triggers other inflammatory signals like IL-1 and IL-6, makes blood vessels leaky, and pulls in more immune cells to the wrong places.
Think of it like a broken smoke detector that won’t stop beeping. TNF inhibitors are the tool that silences it-without turning off your whole house’s power.
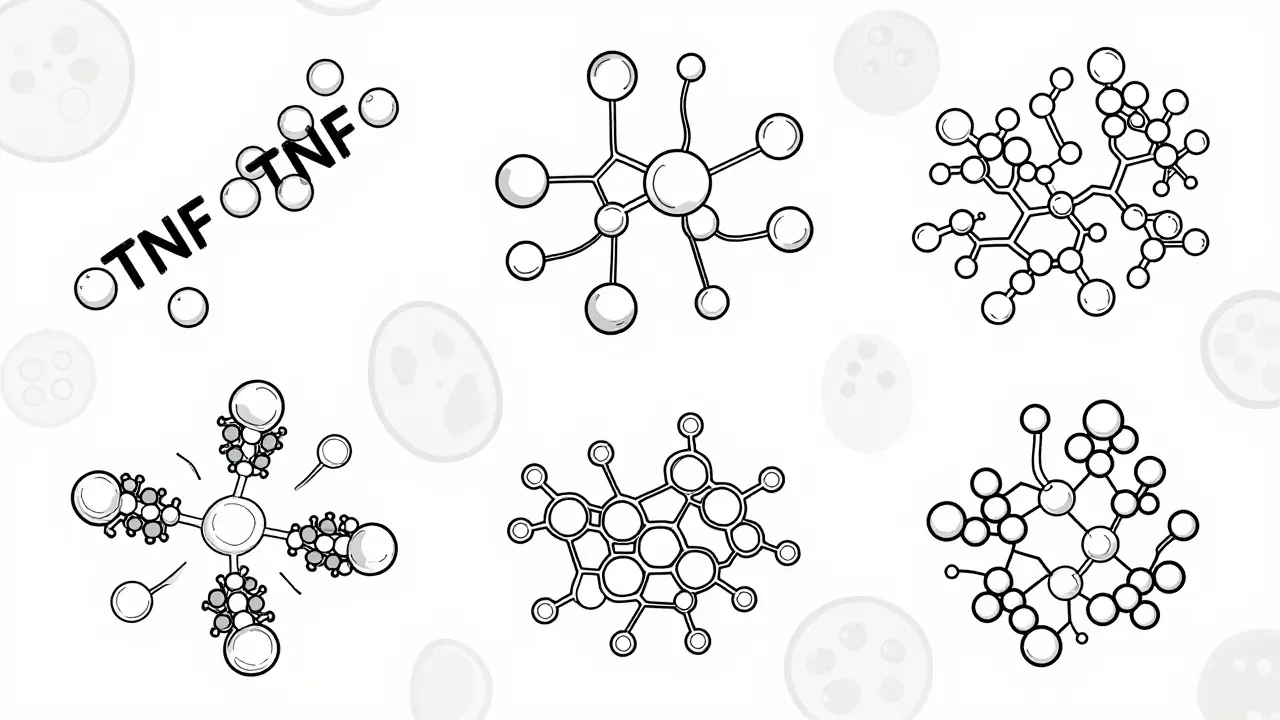
The Five TNF Inhibitors Approved in the U.S.
The U.S. Food and Drug Administration has approved five TNF inhibitors for autoimmune conditions. Each one works differently, and that matters.
- Etanercept (Enbrel) - This one’s a fusion protein. It’s basically a decoy receptor. It looks like part of the TNF receptor your body should have, so TNFα latches onto it instead of your real receptors. It only grabs the floating, soluble version of TNF.
- Infliximab (Remicade) - A full monoclonal antibody. It binds to both floating and cell-bound TNF. It’s given through an IV, usually every 4 to 8 weeks.
- Adalimumab (Humira) - Another monoclonal antibody, but it’s injected under the skin every other week. It’s one of the most prescribed biologics in the world.
- Golimumab (Simponi) - Also a monoclonal antibody, injected monthly. Used mainly for rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis.
- Certolizumab pegol (Cimzia) - Unique because it’s a Fab’ fragment attached to PEG (a polymer). It doesn’t have the Fc portion of an antibody, so it doesn’t trigger immune cell killing. It only binds soluble TNF.
These differences aren’t just technical details. They affect how often you need shots, how your body reacts to them, and even whether you’re at higher risk for certain side effects.
How TNF Inhibitors Actually Work (Beyond Just Blocking)
It’s not as simple as “blocking TNF.” These drugs do more than just sit in your bloodstream and catch TNFα like a net.
Monoclonal antibodies like infliximab and adalimumab can trigger something called antibody-dependent cell-mediated cytotoxicity (ADCC). That means they don’t just neutralize TNF-they help your own immune cells kill the cells that are making too much of it. Think of them as guides that point your immune system to the troublemakers.
Etanercept, on the other hand, doesn’t do that. It just soaks up excess TNF like a sponge. That’s why some doctors think it might be less likely to cause certain side effects, like reactivating latent infections.
There’s also something called reverse signaling. When TNF binds to its receptor on a cell, it can send signals back into that cell. TNF inhibitors can interfere with that too. In some cases, this might help calm down overactive immune cells.
And here’s the twist: TNF isn’t just one thing. It has two main receptors-TNFR1 and TNFR2. TNFR1 drives inflammation and cell death. TNFR2 helps with tissue repair and immune regulation. Some newer research suggests that blocking all TNF might accidentally shut down the good stuff too. That could explain why some people develop new problems-like skin rashes or nerve issues-after starting treatment.
Who Benefits the Most?
TNF inhibitors aren’t first-line drugs. You usually try traditional DMARDs like methotrexate first. If those don’t work-or if your disease is aggressive from the start-then TNF inhibitors come in.
They work best in people with:
- Rheumatoid arthritis with joint damage seen on X-rays
- Psoriatic arthritis with swollen fingers or toes
- Ankylosing spondylitis with stiff spine and chronic back pain
- Moderate to severe Crohn’s disease or ulcerative colitis
- Plaque psoriasis covering more than 10% of the body
Studies show that about 50-60% of rheumatoid arthritis patients see major improvement on TNF inhibitors, compared to only 20-30% on older DMARDs. For some, it’s life-changing. One patient on HealthUnlocked said, “After six months on adalimumab, I went from barely walking to hiking five miles a week.”
But here’s the catch: 30-40% of people eventually lose response. Their body starts making antibodies against the drug. It’s not that the drug stopped working-it’s that their immune system rejected it. This can happen after months or even years. When that happens, switching to another TNF inhibitor might help… or it might not. Sometimes you need to move to a different class of biologic altogether.
The Risks: Infections, Paradoxical Reactions, and More
These drugs suppress part of your immune system. That’s the whole point. But it comes with real dangers.
You’re 2-5 times more likely to get serious infections. Tuberculosis is the big one. That’s why everyone gets a TB skin test or blood test before starting. Even if you had TB as a kid and thought you were fine, it can wake up again.
Fungal infections like histoplasmosis can be deadly if not caught early. That’s why doctors ask about where you’ve lived or traveled-especially in the Midwest or Ohio River Valley in the U.S., or parts of Australia and Africa.
Then there are the paradoxical reactions. Some people develop psoriasis or even multiple sclerosis-like symptoms after starting TNF inhibitors. Why? Because TNF inhibitors can’t cross the blood-brain barrier. So while they calm inflammation in your joints, they might be causing weird imbalances in your nervous system. One 2020 study found patients on TNF inhibitors had more than double the risk of inflammatory brain events.
Injection site reactions are common too-about 20-30% of people get redness, itching, or swelling where they inject. Most fade within days. But for some, it’s a constant annoyance. And the psychological toll of weekly or biweekly shots? That’s real. People talk about it on Reddit forums: the anxiety, the stigma, the feeling of being “marked” by their disease.

What to Expect When You Start
If your doctor says you’re a candidate, here’s what happens next.
First: screening. Blood tests for TB, hepatitis B, and maybe some viral checks. A chest X-ray. You’ll need to be up to date on vaccines-especially flu, pneumonia, and shingles (but not live vaccines).
Then: dosing. If you’re on infliximab, you’ll go to a clinic every 4-8 weeks for a 2-hour IV infusion. Others are self-injected. Etanercept and adalimumab come in pre-filled pens. Most people learn to do it themselves in a week or two. Some need help from a nurse-especially if they have arthritis in their hands.
Manufacturers offer support programs. Humira Complete, for example, gives you 24/7 nurse access, injection training, and help with insurance. Janssen has similar programs for Remicade. These aren’t just perks-they’re critical for sticking with treatment.
You’ll get blood tests every few months to check liver function, blood counts, and signs of infection. Your doctor will ask you: “Any new fevers? Night sweats? Sores that won’t heal?” Don’t downplay symptoms. A small cut that won’t heal could be a sign of something serious.
What Comes After TNF Inhibitors?
TNF inhibitors changed everything. But they’re not the end of the road.
Biosimilars are now widely available. These are near-identical copies of the original drugs. Amjevita, for example, is a biosimilar to Humira. They cost less-sometimes half the price-and work just as well for most people. Many insurers now require you to try a biosimilar first.
And beyond TNF, there are newer biologics. Drugs that target IL-17 (like secukinumab) or IL-23 (like guselkumab) are now first-line for psoriasis. They work faster and sometimes have fewer infection risks.
But TNF inhibitors still hold their ground. For rheumatoid arthritis, Crohn’s, and ankylosing spondylitis, they’re often the most proven option. And for many, they’re the only thing that worked.
The future? More targeted drugs. Researchers are working on agents that block only TNFR1-the bad actor-while leaving TNFR2 alone. That could mean the same benefits, without the paradoxical side effects. Early trials are promising.
Final Thoughts: It’s Not One-Size-Fits-All
TNF inhibitors are powerful. They’ve given millions of people back their lives. But they’re not a cure. They’re a tool. And like any tool, they need to be used carefully.
If you’re considering one, ask your doctor: Why this one? What’s the plan if it stops working? What are the signs of trouble? And what happens if I get sick?
There’s no shame in needing help. Autoimmune disease doesn’t care how strong you are. But with the right treatment, you can still live well-on your terms.








14 Comments