Why Your Prescription Label Matters More Than You Think
Every time you pick up a new prescription, you’re handed a small piece of paper that could save your life-or hurt you if you don’t understand it. It’s not just a receipt. It’s your instruction manual for something powerful: medicine. And yet, most people glance at it, shove it in their bag, and hope for the best. That’s risky. Around 79% of patients misread at least one part of their prescription label, according to NIH research. Some think “twice daily” means every two hours. Others take expired pills because they didn’t check the date. These mistakes aren’t rare. They’re common. And they lead to hospital visits, bad reactions, and even death.
What’s on Your Prescription Label? The 12 Key Parts
Don’t just look at the name and dose. Every prescription label has 12 essential pieces of information. Missing one could mean taking the wrong thing, at the wrong time, in the wrong way.
- Patient name - This is your full legal name. If it says “John Smith” and you’re Jane Smith, don’t take it. This is the first line of defense against mix-ups, especially in households where multiple people take pills.
- Medication name - You’ll see both the brand name (like “Lipitor”) and the generic name (like “atorvastatin”). In Australia and Canada, the generic name comes first. Always check both. If the pill looks different from your last refill, ask why.
- Prescription number (Rx#) - This is your prescription’s ID. Use it when calling for refills. If you can’t find it, the pharmacy can look you up, but having it saves time.
- Prescriber name - Who ordered this? Your GP? A specialist? A dentist? Knowing this helps if you need to follow up or if something goes wrong.
- Medication strength - This tells you how much medicine is in each pill or drop. “20 mg” means 20 milligrams per tablet. If your last prescription was 10 mg and now it’s 20 mg, confirm with the pharmacist. Don’t assume it’s a mistake.
- Quantity - How many pills, milliliters, or grams are in the bottle? If you got 30 tablets but the label says “take one daily,” that’s a month’s supply. If you got 10 tablets for a 30-day course, something’s off.
- Discard/expiration date - Most prescriptions expire one year after being filled. After that, the medicine might not work-or it could break down into something harmful. Never take pills past this date.
- Instructions - This is where most people get confused. “Take one tablet by mouth twice daily” means two times a day, not every 12 hours unless specified. “Take with food” means eat something before or after. “Take on an empty stomach” means no food for two hours before or after. Don’t guess. If it says “as needed,” ask what that means for your condition.
- Refill info - How many more times can you get this without a new prescription? “Refills: 3” means you can get it three more times. After that, your doctor must approve another one.
- Auxiliary labels - These are the small stickers: “May cause drowsiness,” “Avoid alcohol,” “Refrigerate,” “Shake well.” These aren’t optional. They’re safety rules. Ignoring “Avoid sunlight” on a tetracycline label could give you a bad burn.
- Pharmacy info - Name, phone number, address. Keep this. If you have questions, call them. Pharmacists are trained to explain labels. They want you to understand.
How to Spot a Misunderstood Instruction
Some phrases sound simple but trip people up every time.
- “Twice daily” - Not “every 12 hours.” It means morning and night, roughly 12 hours apart. But if you’re sleeping through the night, taking it at breakfast and dinner is fine.
- “Every 8 hours” - This means exactly that. Set an alarm. Don’t just take it when you remember.
- “As needed” - This is dangerous without context. “As needed for pain” means take it only when you feel pain-not every hour. “As needed for anxiety” might mean one dose per day, max. Ask for specifics.
- “Take with food” - Does that mean during the meal? Right after? The label doesn’t say. Ask your pharmacist. Some meds need food to avoid stomach upset. Others need food to absorb properly.
- “Take on an empty stomach” - This means no food for 1 hour before and 2 hours after. That’s a long time. Plan your doses around meals.
Research shows patients with low health literacy are over twice as likely to misread these instructions. Even people who read well can get tripped up by vague wording. That’s why you should never assume.

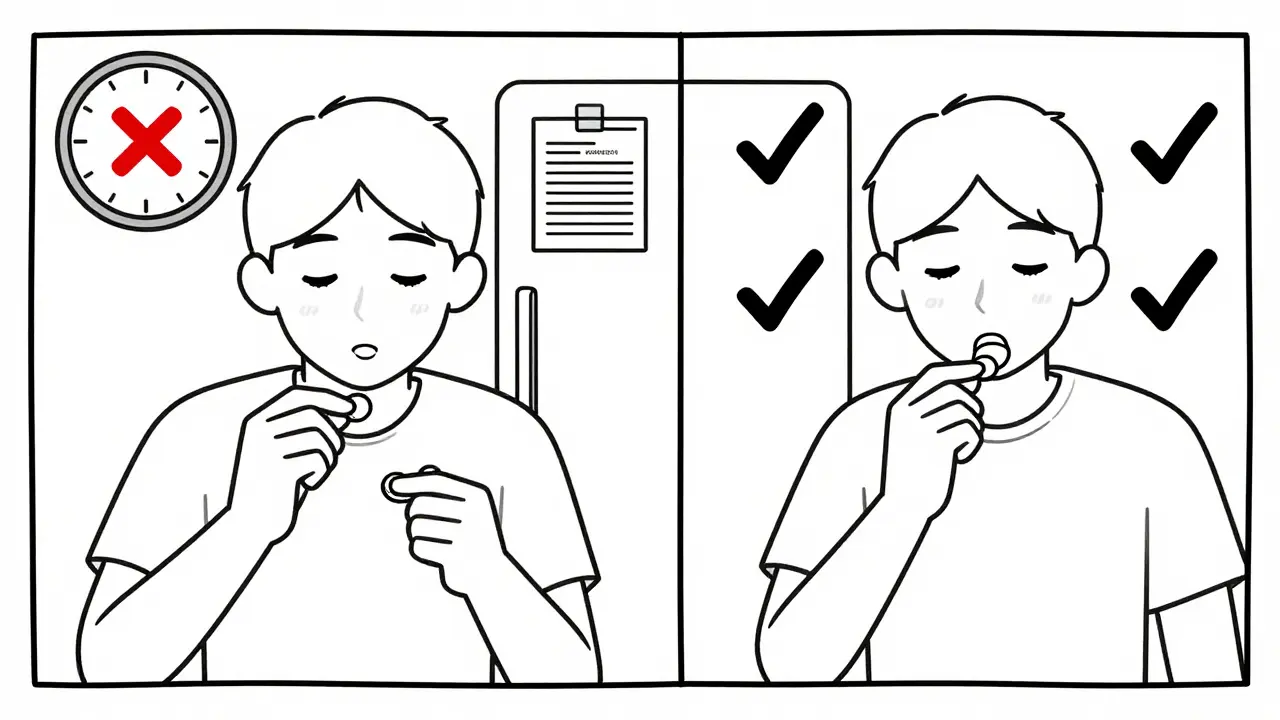
What to Do Before You Take Any Pill
Make this a habit. Before you swallow anything, run through this quick checklist:
- Check your name - Is it really yours? No nicknames, no initials.
- Match the pill - Does it look like the last one you took? Same color? Same shape? Same imprint? If not, ask why.
- Confirm the strength - Is it the same dose as before? If your blood pressure med changed from 25 mg to 50 mg, that’s a big jump. Double-check.
- Read the instructions out loud - Say them to yourself. Then say them to someone else. If they don’t make sense, the label might be unclear.
- Look for auxiliary labels - Did you miss the “Avoid alcohol” sticker? That’s a red flag.
- Check the expiration date - If it’s expired, return it. Don’t risk it.
- Know who to call - Write down the pharmacy’s number. Keep it on your fridge or phone.
Spending just two minutes on this every time you get a new prescription cuts your risk of a bad reaction by over 60%. That’s not a guess. That’s data from the FDA and the Institute of Medicine.
When to Ask for Help
You don’t have to figure this out alone. Pharmacists are there to help. Don’t feel embarrassed to say: “I’m not sure what this means.”
- Ask for a printed copy of the instructions in plain language.
- Request a verbal explanation. Say, “Can you walk me through this like I’ve never taken medicine before?”
- Ask if there’s a video or app that explains it. Some pharmacies in Australia now offer QR codes on labels that link to short videos in multiple languages.
- If you’re visually impaired, ask for a large-print label or audio instructions.
- If English isn’t your first language, ask for an interpreter. This is your right.
Pharmacies in Sydney and across Australia are required to provide clear communication. If they don’t, ask for the manager. You’re not being difficult-you’re protecting your health.
What Happens When You Get It Wrong
Medication errors cause 1.5 million preventable injuries in the U.S. every year. That’s one every 22 seconds. In Australia, the numbers are similar. Many of these happen because someone took the wrong dose, the wrong pill, or took it at the wrong time.
One woman took her blood thinner twice because she thought “twice daily” meant every 12 hours-so she took one at 7 a.m. and another at 7 p.m. But her prescription said “take one tablet daily.” She ended up in the ER with internal bleeding.
A man with diabetes took his insulin at breakfast because the label said “take with food.” He didn’t realize “take with food” meant only if he was eating. He took it on an empty morning and went into a coma.
These aren’t outliers. They’re preventable.
What’s Changing on Prescription Labels
Labels are getting better. In 2014, the FDA pushed for clearer language. Now, labels avoid terms like “bid” or “q.d.” and use “twice daily” and “once daily.”
In Australia, the Therapeutic Goods Administration (TGA) now requires standardized auxiliary labels. That means “Avoid Alcohol” looks the same on every prescription, no matter which pharmacy you use.
By 2025, most Australian pharmacies will offer digital labels through apps. You’ll scan a QR code and get a video in your language, with animations showing how to take the pill, what to avoid, and what side effects to watch for.
But until then, the paper label is still your main tool. And it’s your responsibility to read it.
Your Prescription Label Is Your Safety Net
Medicine is powerful. It can heal. But it can also harm-if you don’t know how to use it. Reading your prescription label isn’t just smart. It’s essential. It’s the difference between getting better and ending up in the hospital.
Don’t trust memory. Don’t guess. Don’t assume. Take two minutes. Read every line. Ask questions. Call the pharmacy. Write it down. Do it every time. Your life depends on it.
What should I do if my prescription label looks different from last time?
Don’t take it until you’ve checked with your pharmacist. Even small changes in color, shape, or size can mean a different drug or strength. Always confirm the medication name, strength, and instructions match what your doctor prescribed. If something’s off, the pharmacy may have made a mistake-or switched to a generic version. Either way, ask before you take it.
Can I take medicine past the expiration date?
No. Most medications lose effectiveness after one year from the date they were dispensed. Some, like insulin or liquid antibiotics, can become dangerous. Even if it looks fine, it might not work. Expired pills won’t kill you immediately, but they won’t treat your condition either. Return expired meds to your pharmacy for safe disposal.
What does “take with food” really mean?
It means eat something-any food-before or after taking the pill. You don’t need a full meal. A cracker, banana, or glass of milk is enough. This helps your stomach absorb the drug properly and reduces nausea or upset. But don’t take it right before bed if you’re not eating. Ask your pharmacist for exact timing if you’re unsure.
Why does my label have a DIN or NDC number?
The DIN (Drug Identification Number) is Australia’s unique code for each medicine, assigned by the Therapeutic Goods Administration. The NDC is the U.S. equivalent. These numbers help track the drug’s manufacturer, strength, and form. You don’t need to remember them, but they’re useful if you need to report a side effect or check if your medicine is recalled.
Can I split or crush my pills if they’re hard to swallow?
Only if the label or your pharmacist says it’s okay. Some pills are designed to release medicine slowly. Crushing them can release the full dose at once, which can be dangerous. Others have coatings to protect your stomach. Always ask before altering your pills.
How do I know if I’m having a bad reaction?
Watch for sudden rashes, swelling, trouble breathing, chest pain, extreme dizziness, or confusion. These are signs of a serious reaction. Call emergency services immediately. For milder side effects like nausea or drowsiness, check the auxiliary label. If it’s listed, it’s normal. If it’s not, call your pharmacist or doctor.
Next Steps: Make This a Routine
Start today. When you get your next prescription, don’t rush out the door. Sit down. Read every word. Ask one question. Write down the answer. Keep the label in a visible spot-on your fridge, next to your toothbrush, or taped to your pill organizer. Make reading it part of your daily routine, like brushing your teeth.
And if you’re helping someone else-your parent, partner, or friend-do it with them. Talk through the label. Explain it in your own words. You might be the reason they stay safe.








8 Comments