Antifungals Can Hurt Your Liver - Here’s How to Stay Safe
Most people think of antifungals as simple pills for athlete’s foot or nail fungus. But when taken systemically - especially for serious infections - these drugs carry real, sometimes deadly, risks to your liver. You might not feel sick at first. No nausea. No jaundice. Just a little fatigue. Then, weeks later, your liver enzymes spike. Sometimes, it’s too late.
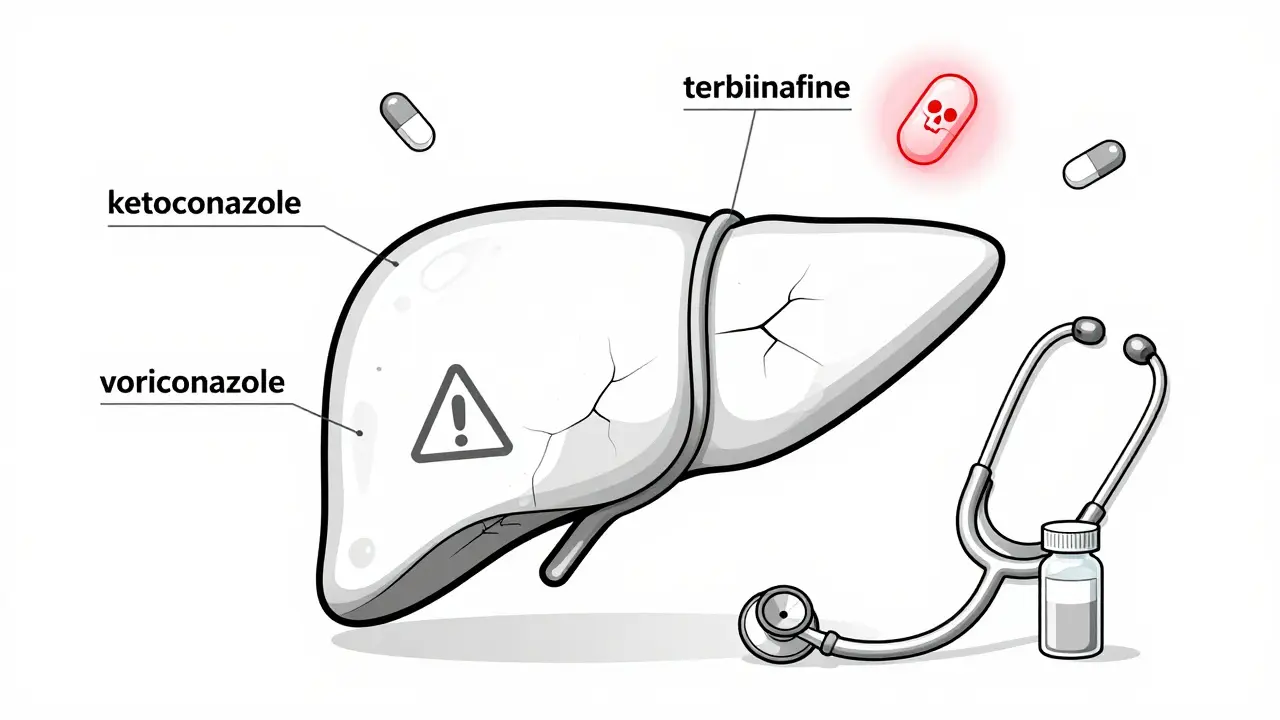
The truth? Not all antifungals are created equal. Some, like ketoconazole, are so dangerous they’ve been pulled from shelves in Europe and restricted in the U.S. Others, like terbinafine, are safer but still carry black box warnings. And then there’s voriconazole and itraconazole - the ones doctors reach for in hospitals, but with strict monitoring rules because they’re linked to more liver injuries than any other antifungal class.
Which Antifungals Are Most Dangerous for Your Liver?
The FDA’s adverse event database from 2004 to 2021 shows a clear pattern: azoles are the biggest culprits. Among them, itraconazole and voriconazole stand out. In one analysis, voriconazole was tied to more than 900 reports of liver injury - more than fluconazole by a factor of three. Ketoconazole, once a common treatment for fungal infections, had the most severe warnings. It’s now banned in Europe and restricted in the U.S. to only the most desperate cases because of its high risk of sudden, life-threatening liver failure.
Even the "safer" azoles aren’t risk-free. Fluconazole is often chosen for its lower liver toxicity, but that doesn’t mean it’s harmless. In patients on long-term therapy - say, for recurring candidiasis - liver damage can still occur. The key is timing. Most liver injury from azoles shows up between 2 and 8 weeks after starting treatment. That’s why weekly blood tests are required during the first month.
Terbinafine, used mostly for nail fungus, has the lowest absolute risk - around 0.1% of users. But here’s the catch: it can still cause liver failure. One patient in Australia reported jaundice at week five. Their bilirubin hit 12.3 mg/dL - over ten times the normal level. They spent three weeks in the hospital. Terbinafine’s black box warning exists for a reason.
Echinocandins like caspofungin and micafungin were once thought to be liver-friendly. But newer data shows they’re not innocent. Anidulafungin had the highest death rate among DILI cases in the FDA database - 50%. That sounds terrifying, but it’s likely because these drugs are given to the sickest patients - those already in liver failure. Micafungin, by contrast, has the cleanest safety record among echinocandins.
Why Do Some People Get Liver Damage and Others Don’t?
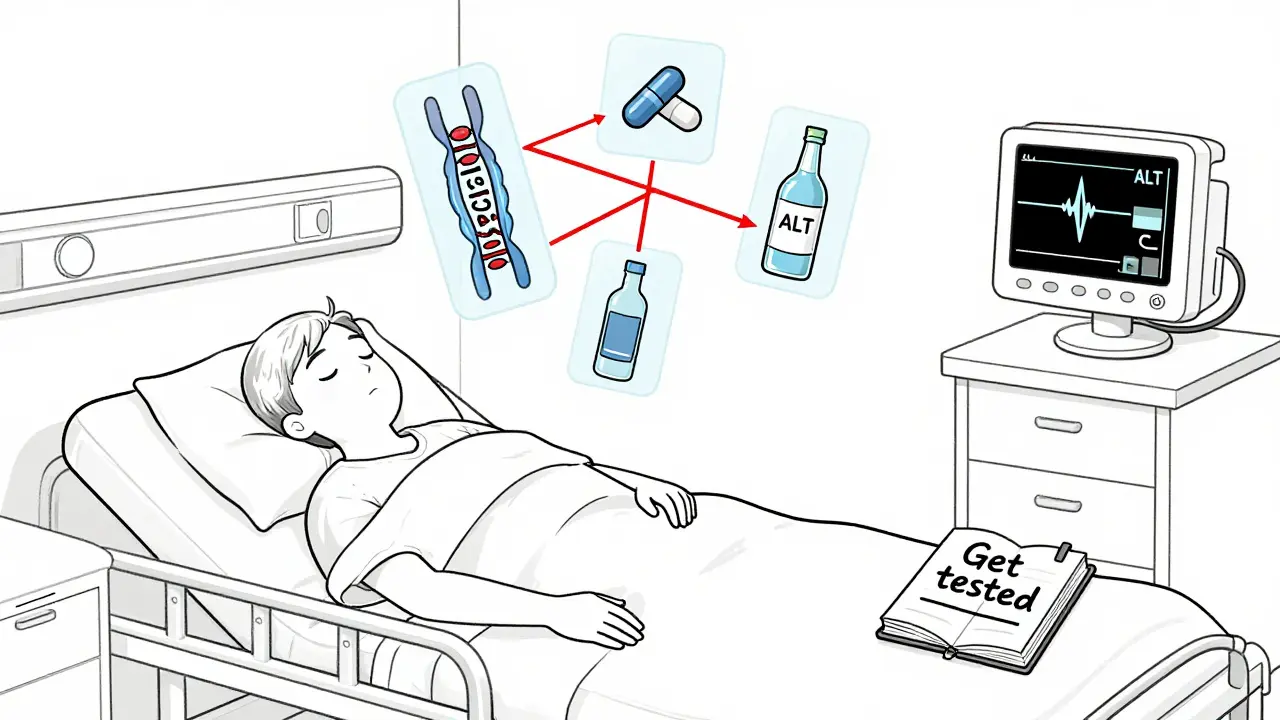
It’s not just the drug. It’s your genes. In 2022, researchers found that people with a specific variation in the CYP2C19 gene - common in about 20% of the population - are 3.7 times more likely to suffer liver injury from voriconazole. This isn’t theoretical. It’s measurable. Hospitals in Sydney and Melbourne are now starting to test for this before prescribing voriconazole to high-risk patients.
Age matters too. People over 65 are nearly eight times more likely to develop antifungal-induced liver injury than younger adults. And if you’re on other meds - especially statins, seizure drugs, or even some antibiotics - your risk goes up. Antifungals interfere with liver enzymes (CYP3A4, CYP2C9, CYP2C19) that break down dozens of other drugs. A simple interaction can turn a safe dose into a toxic one.
One real case from a Sydney GP: a 71-year-old man on simvastatin for cholesterol started terbinafine for toenail fungus. Two weeks later, he was admitted with ALT levels over 1,500 U/L. He didn’t know the two could interact. His doctor didn’t check. He recovered after stopping both drugs, but it took months.
What Symptoms Should You Watch For?
Liver damage from antifungals doesn’t always show up on a blood test before you feel it. Early signs are vague - the kind of symptoms you might ignore:
- Unexplained fatigue that doesn’t improve with rest
- Nausea or loss of appetite
- Dark urine
- Yellowing of the skin or eyes (jaundice)
- Pain or swelling under your right ribs
- Itchy skin without a rash
These aren’t emergencies on their own. But if you’re on an antifungal and notice even one of these, stop the drug and get your liver checked immediately. Don’t wait. Don’t assume it’s "just a virus."
Monitoring Is Non-Negotiable
If you’re prescribed a systemic antifungal, you need blood tests. Not optional. Not "if you feel off."
The Infectious Diseases Society of America says:
- Baseline LFTs before starting any systemic antifungal
- Weekly tests for the first month for high-risk drugs (voriconazole, itraconazole, ketoconazole)
- Biweekly after that until treatment ends
- For terbinafine: test at 4-6 weeks, then every 4-8 weeks if treatment lasts longer than 8 weeks
Here’s when to stop: if your ALT or AST levels hit 3 times the upper limit of normal AND you have symptoms - stop immediately. If they hit 5 times normal without symptoms - still stop. No exceptions. The goal isn’t to finish the course. It’s to avoid liver failure.
But here’s the problem: a 2020 study found only 37% of primary care doctors actually monitor LFTs during terbinafine therapy. Most think it’s safe because it’s "just for nails." It’s not. If your doctor doesn’t offer a blood test before or during treatment, ask for one. Politely but firmly.
What About Over-the-Counter Antifungals?
Topical creams, sprays, and shampoos for athlete’s foot or dandruff? They’re safe. Very little gets absorbed into your bloodstream. No liver risk.
But oral antifungals sold online without a prescription? That’s where things get dangerous. In Australia, it’s illegal to sell oral ketoconazole without a prescription - but it still shows up on dark web pharmacies. People buy it for yeast infections or acne, thinking it’s a miracle cure. Then they end up in the ER with acute liver failure.
Don’t risk it. If you need an oral antifungal, see a doctor. Get tested. Get monitored. There’s no shortcut.
What’s Changing in Antifungal Treatment?
The tide is turning. Hospitals are using echinocandins like micafungin as first-line for invasive candidiasis - not because they’re perfect, but because they’re safer for the liver than azoles in critically ill patients.
New drugs like olorofim and ibrexafungerp are in development. Early trials show they cause 78% fewer liver enzyme spikes than older azoles. That’s huge. These drugs may become the new standard within the next five years.
Meanwhile, AI is being added to the FDA’s adverse event database to catch liver injury signals faster. In 2024, a pilot program will flag patients at risk before they even hit the hospital.
But for now? The rules are simple: know your drug. Know your risk. Get tested.
What If You’ve Already Taken an Antifungal?
If you took terbinafine, itraconazole, or voriconazole in the last six months and didn’t get liver tests, get them now. Even if you feel fine. Liver damage can be silent.
If you had a reaction - elevated enzymes, jaundice, fatigue - tell your doctor. Write it down. Include the drug name, dose, and when you took it. That information helps future patients.
And if you’re still on one? Don’t stop cold turkey without talking to your doctor. But do ask: "Is this the safest option for my liver? Do I need blood work?"
Antifungals save lives. But they can also end them - quietly, without warning. The difference between safety and disaster is often just a blood test and a conversation.
Can antifungals cause permanent liver damage?
Yes, in rare cases. Most liver injury from antifungals reverses after stopping the drug. But in about 5-10% of severe cases, especially with ketoconazole or delayed diagnosis, patients develop acute liver failure requiring transplant. Early detection is the only way to prevent this.
Is fluconazole safer than other azoles?
Yes, fluconazole has the lowest risk of liver injury among azoles. But it’s not risk-free. For short-term use (under 2 weeks), monitoring isn’t usually needed. For longer courses - like treating chronic candidiasis - baseline and periodic liver tests are recommended, especially in older adults or those on other medications.
Can I drink alcohol while taking antifungals?
No. Alcohol stresses the liver and increases the risk of drug-induced injury. This is especially dangerous with ketoconazole, itraconazole, and voriconazole. Even moderate drinking can push your liver into failure. Avoid alcohol completely while on these drugs and for at least two weeks after stopping.
Why was ketoconazole pulled from the market?
Ketoconazole was withdrawn in Europe in 2013 and restricted in the U.S. because it caused severe, sometimes fatal, liver injury in 1 in 500 users. It also disrupted adrenal hormone production and had dangerous interactions with many common drugs. Safer alternatives exist, so its risks no longer outweigh its benefits.
Should I get genetic testing before taking voriconazole?
If you’re at high risk - over 65, on multiple medications, or have a history of liver issues - genetic testing for CYP2C19 variants is becoming standard in major hospitals. It’s not yet routine everywhere, but it can cut your liver injury risk by more than 70%. Ask your infectious disease specialist if it’s right for you.








8 Comments