Diabetes Medication Comparison Tool
Your Health Priorities
Select the health factors most important to you. The tool will show which diabetes medication best matches your priorities.
Key Takeaways
- Dapasmart is an SGLT2 inhibitor that lowers blood sugar and offers heart‑kidney protection.
- Jardiance (empagliflozin) provides the strongest cardiovascular benefit, while Invokana (canagliflozin) has the highest HbA1c reduction.
- Cost and PBS listing vary: Farxiga is PBS‑subsidised, Dapasmart often requires private purchase.
- Common side‑effects across the class include genital infections and mild dehydration; rare ketoacidosis needs monitoring.
- Choosing the right drug depends on your cardiovascular risk, kidney function, budget, and tolerance to side‑effects.
What is Dapasmart and how does it work?
When you see the name Dapasmart is a brand‑name tablet that contains the active ingredient dapagliflozin, an SGLT2 (sodium‑glucose co‑transporter‑2) inhibitor. By blocking SGLT2 in the kidney, it forces excess glucose to leave the body through urine, lowering blood‑sugar levels without increasing insulin.
Dapagliflozin belongs to the broader class SGLT2 inhibitor. Besides glucose control, the drug improves heart failure outcomes and slows chronic kidney disease progression - benefits established in the DAPA‑CKD and DAPA‑HF trials (2019‑2022).
How does Dapasmart compare on efficacy?
The primary measure clinicians look at is HbA1c reduction after 24 weeks of therapy. Dapasmart typically drops HbA1c by 0.7‑0.9% when added to metformin. Below is a side‑by‑side view of three popular alternatives.
| Medication | Active Ingredient | Typical HbA1c Reduction | Cardiovascular Benefit | Renal Benefit |
|---|---|---|---|---|
| Dapasmart | dapagliflozin | 0.7‑0.9% | ↓ 12% major adverse cardiovascular events (MACE) | ↓ 39%eGFR decline |
| Jardiance | empagliflozin | 0.6‑0.8% | ↓ 14% MACE, strongest heart‑failure reduction | ↓ 34%eGFR decline |
| Invokana | canagliflozin | 0.9‑1.0% | ↓ 10% MACE | ↓ 40%eGFR decline |
| Farxiga | dapagliflozin (same active as Dapasmart) | 0.7‑0.9% | ↓ 12% MACE | ↓ 39%eGFR decline |
Notice that Farxiga mirrors Dapasmart’s numbers because they share the same molecule. The slight edge in HbA1c for Invokana comes with a higher amputation warning, which we’ll discuss next.
Safety profile - what side‑effects should you watch?
All SGLT2 inhibitors share a core set of adverse events:
- Genital mycotic infections (5‑10% of users)
- Urinary tract infections (UTIs) - slight increase compared with placebo
- Volume depletion - especially in older adults on diuretics
Specific differences emerge:
- Invokana carries a boxed warning for lower‑leg amputation, observed in the CANVAS program (≈0.2% higher risk).
- Jardance (empagliflozin) reports the lowest rate of genital infections (<5%).
- Dapasmart and Farxiga have comparable infection rates, but Dapasmart may be less available under the Australian PBS, leading some patients to self‑pay and possibly miss early monitoring.
Rare but serious: euglycaemic diabetic ketoacidosis (DKA). Incidence across the class is <0.2% but rises when patients are on a very low‑carb diet or have acute illness. The key is education - stop the drug during surgery, severe illness, or prolonged fasting.
Cost, PBS listing and practicality in Australia
Pricing matters. As of October2025:
- Farxiga is listed on the Australian Pharmaceutical Benefits Scheme (PBS) for type2 diabetes with a $12.50 co‑payment per month.
- Dapasmart is not PBS‑subsidised; a 30‑day pack costs roughly AUD$70‑$80 out‑of‑pocket.
- Jardiance entered the PBS in 2024 for patients with established cardiovascular disease; co‑payment is $25 per month.
- Invokana is PBS‑eligible for chronic kidney disease with a similar $25 co‑payment, but the amputation warning limits its use in patients with peripheral vascular disease.
If you have private health cover, the gap may shrink, but the out‑of‑pocket burden still leans toward Farxiga for most Australians without a specific indication for Jardiance or Invokana.
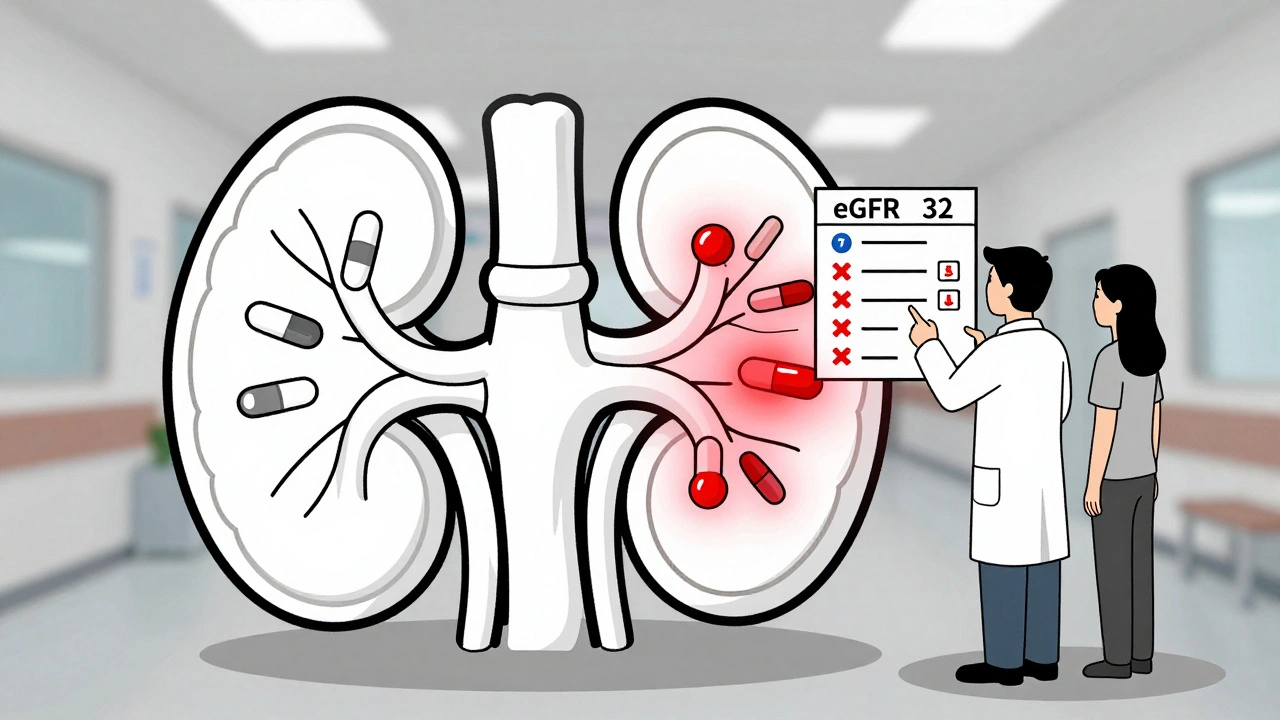
How to pick the right drug for your situation
Think of the decision as a simple flow:
- Do you have heart failure or established atherosclerotic cardiovascular disease (ASCVD)? If yes, Jardiance has the strongest heart‑failure data; Dapasmart/Farxiga still help but Jardiance wins the cardio‑outcome race.
- Is kidney function declining (eGFR 30‑60mL/min/1.73m²)? All four agents slow decline, but dapagliflozin (Dapasmart/Farxiga) has the most robust renal‑outcome trial (DAPA‑CKD).
- Are you at risk for amputation or have peripheral artery disease? Avoid Invokana.
- What is your budget? PBS‑subsidised options (Farxiga, Jardiance, Invokana) are generally cheaper than Dapasmart.
- Do you tolerate genital infections? If infections are a concern, Jardiance may be gentler.
Combine these checks with your doctor’s assessment of other meds, like metformin, sulfonylureas, or GLP‑1 agonists (e.g., Ozempic). Adding an SGLT2 inhibitor to a GLP‑1 agonist can push HbA1c down 1.5‑2% total, but watch for overlapping gastrointestinal side‑effects.

Real‑world example: Sam’s switch from metformin alone to a combo
Sam, a 58‑year‑old Sydney resident, was on metformin 1g twice daily with an HbA1c of 8.3%. His doctor noted early kidney decline (eGFR55) and mild heart‑failure symptoms. Sam chose Dapasmart (private) because he wanted the renal data from DAPA‑CKD and wasn’t eligible for PBS‑subsidy yet. After three months, his HbA1c fell to 7.4% and eGFR stabilized. He reported two mild yeast infections, treated with topical azoles, and none of the volume‑depletion symptoms. Six months later, Sam switched to Farxiga once PBS covered it, saving $60 per month without losing efficacy.
Bottom line
If cardiovascular protection is your top priority and you qualify for PBS, Jardiance is the clear pick. If kidney protection and broad affordability matter, Farxiga (the PBS version of dapagliflozin) beats Dapasmart on price while delivering identical efficacy. Invokana may be best for those needing the biggest HbA1c dip and without peripheral disease. Dapasmart remains a solid option for patients who prefer a private brand or need a specific dosage not yet listed on PBS.
Frequently Asked Questions
Can I take Dapasmart with insulin?
Yes, dapagliflozin can be combined with basal or bolus insulin. The insulin dose often needs reduction (10‑20%) to avoid hypoglycaemia, especially if you’re also on sulfonylureas.
Is Dapasmart safe for people with a history of urinary infections?
A history of recurrent UTIs raises the risk, but many patients continue the drug with close monitoring and increased hydration. Discuss with your doctor before starting.
How long does it take to see a drop in HbA1c?
Most trials show a statistically significant reduction by 12weeks, with the maximal effect around 24‑26weeks.
Do I need to stop Dapasmart before surgery?
Yes, stop at least 48hours before any elective surgery or major procedure to lower the risk of ketoacidosis.
What if I’m pregnant or planning pregnancy?
SGLT2 inhibitors, including dapagliflozin, are not recommended during pregnancy due to limited safety data. Switch to insulin or metformin under medical guidance.







12 Comments