When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version. But how does the FDA make sure it does? The answer lies in a quiet but powerful lab test called dissolution testing. This isn’t just paperwork-it’s the backbone of trust in every generic drug you take.
What Dissolution Testing Actually Does
Dissolution testing measures how quickly a drug releases its active ingredient in a controlled lab environment. Imagine putting a pill in a beaker of fluid that mimics your stomach. The test tracks how much of the drug dissolves over time. If the generic dissolves at the same rate as the brand-name drug, it’s likely to behave the same inside your body. No need for expensive and risky human trials every time.
The FDA doesn’t just ask for this data-they demand it. For any oral solid dose drug-tablets, capsules, or suspensions-dissolution testing is mandatory. That means nearly every generic you buy has passed this test. Drugs already in liquid form, like syrups or eye drops, don’t need it because they’re already dissolved. But anything you swallow as a solid? It gets tested.
The Five Pillars of FDA Dissolution Requirements
The FDA doesn’t leave room for guesswork. Generic drug makers must submit five types of dissolution data before approval:
- Solubility of the active ingredient-How well does the drug dissolve in water or stomach fluid?
- Test method validation-What equipment was used? What pH? How much fluid? At what speed? (Most use USP Apparatus 1 or 2, spinning at 50-100 rpm.)
- Method robustness-What happens if you tweak the temperature, pH, or rotation speed? The method must still work.
- Analytical accuracy-Can the lab reliably measure how much drug is dissolved? No guesswork allowed.
- Discriminatory power-Can the test tell the difference between a good and bad formulation? This is critical for slow-release pills or hard-to-dissolve drugs.
Each of these points is backed by data. One wrong assumption, and the application gets rejected. No shortcuts.
How Fast Must the Drug Dissolve?
There’s no one-size-fits-all number. But here’s the baseline: for most immediate-release tablets, at least 80% of the drug must dissolve within 45 minutes. For highly soluble drugs (BCS Class I), the FDA simplified this. If the drug dissolves quickly and absorbs well, a single test at 30 minutes in 900 mL of 0.1N HCl is enough. That’s it. No extra time points. No complex curves. Just one clean result.
For slower-release pills-like those designed to last 12 hours-the test gets harder. The FDA requires testing under multiple pH levels (1.2, 4.5, and 6.8) to mimic different parts of your gut. And here’s something most people don’t know: they also test with alcohol. Yes, alcohol. Why? Because if someone takes a slow-release pill with a drink, the drug could dump all at once-called dose-dumping. That’s dangerous. Dissolution testing catches this before the drug hits shelves.
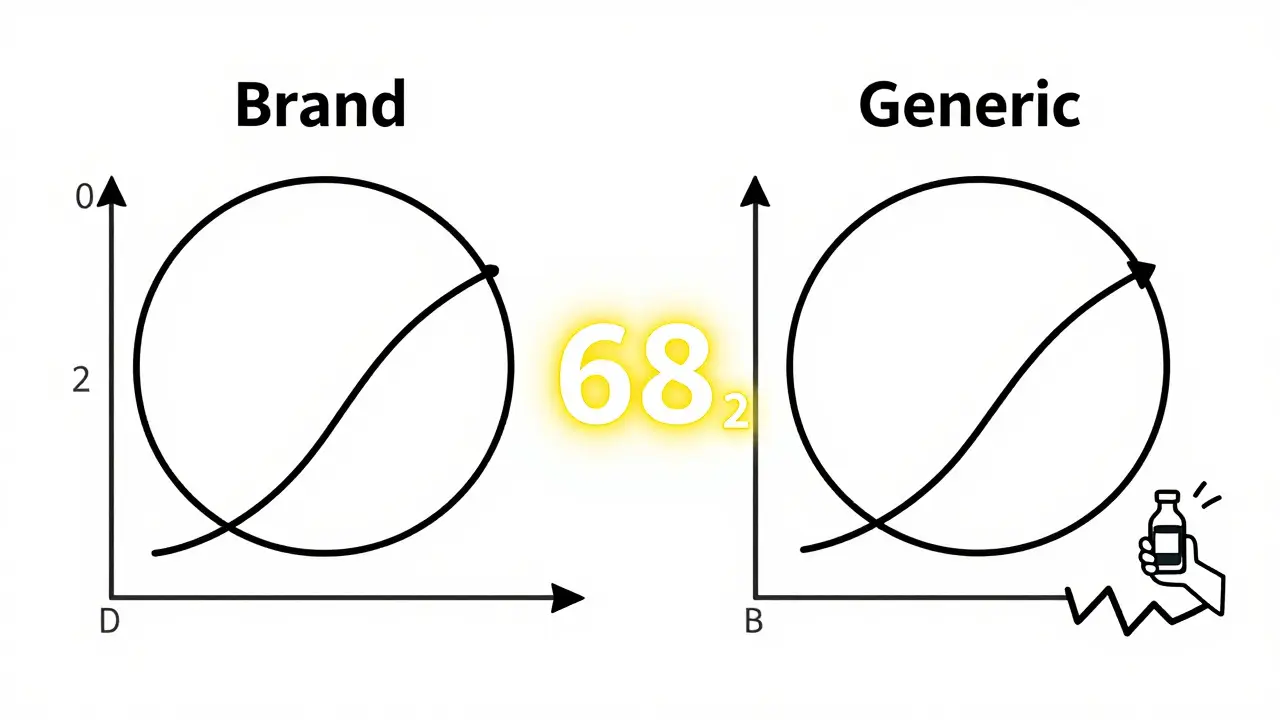
The f2 Similarity Factor: The Math Behind Equivalence
How do you prove two pills dissolve the same way? It’s not just about matching numbers at one time point. The FDA uses a statistical tool called the f2 similarity factor. Think of it like a match score between two dissolution curves.
The formula compares how both the generic and brand-name pills dissolve over time. If the f2 score is 50 or higher, the FDA considers them equivalent. A score below 50? You need to fix the formula. A score above 85? You’re in the clear. This isn’t a soft guideline-it’s a hard rule written into the approval process.
For example, if a brand-name pill releases 20% at 15 minutes, 50% at 30 minutes, and 85% at 60 minutes, the generic must follow that same pattern. Not close. Not almost. Exactly that pattern.
Why This Matters More Than You Think
Dissolution testing isn’t just about safety-it’s about access. Before this system, every generic drug needed human bioequivalence studies. That meant dozens of volunteers, weeks of monitoring, and costs that could top $1 million per drug. Dissolution testing cuts that down to a few weeks in a lab. That’s why generic drugs are 80-85% cheaper than brand names.
For the FDA, this test is a diagnostic tool. If a manufacturer changes the pill’s coating, switches suppliers, or tweaks the manufacturing line, they must retest dissolution. If the curve changes, the FDA halts production. No exceptions. This is how a pill made in India, Mexico, or Ohio ends up identical to the one made in New Jersey.
And it works. The FDA’s Dissolution Methods Database contains over 2,800 approved methods for specific drugs. Manufacturers use this like a recipe book. If your drug is listed, you follow the method. If it’s not, you build one from scratch-and prove it works.
Where the System Gets Tough
Not all drugs are easy to test. Low-solubility drugs-like those used for cancer or epilepsy-are tricky. They don’t dissolve well, even in the best conditions. For these, the FDA demands extra steps: multiple media, different temperatures, even surfactants to help the drug dissolve. The method must be able to spot tiny differences between batches. One bad batch could mean a patient doesn’t get enough medicine.
Developing a reliable dissolution method for these drugs can take 6 to 12 months. Companies spend months tweaking buffers, rotation speeds, and sampling times. One wrong choice, and the whole application stalls. That’s why many generic makers hire specialists just for dissolution testing.
Documentation is another hurdle. The ANDA submission includes 50 to 100 pages of dissolution data alone. Every instrument calibration, every buffer recipe, every run is recorded. The FDA reviews every line. No room for sloppy notes.
What’s Next for Dissolution Testing?
The FDA is moving toward more realistic testing. Right now, most tests use simple buffers. But your gut isn’t a beaker. Researchers are testing methods that simulate real stomach acid, food effects, and even gut motility. The goal? Make lab results better predict real-world performance.
There’s also talk of expanding biowaivers. Right now, only BCS Class I drugs (high solubility, high permeability) can skip human studies. But early data suggests BCS Class III drugs (high solubility, low permeability) might qualify too. If approved, this could cut approval times for dozens more drugs.
By 2025, experts expect 35% of generic approvals to rely on standardized dissolution methods-up from 25% in 2020. That means more affordable drugs, faster. But the FDA won’t sacrifice quality. Every method still must be product-specific. No cookie-cutter rules.
Final Thought: Trust, But Verify
You don’t need to understand the math or the machines. But you should know this: every generic pill you take has been tested to prove it works like the brand. That’s not luck. It’s science. It’s regulation. It’s thousands of hours of lab work, backed by data, enforced by the FDA. That’s why you can trust a $5 pill as much as a $50 one.
What drugs require dissolution testing?
Dissolution testing is required for all oral solid dose drugs-tablets, capsules, and suspensions-and oral semi-solid products. It’s not needed for drugs already in solution, like oral liquids, eye drops, or topical gels, because they don’t need to dissolve in the body.
How does the FDA decide if a generic drug is equivalent?
The FDA uses the f2 similarity factor, a statistical tool that compares the dissolution profile of the generic drug to the brand-name drug. If the f2 score is 50 or higher, the two are considered equivalent. This means the drug releases at the same rate and extent under the same test conditions.
Can a generic drug be approved without human trials?
Yes. For drugs classified as BCS Class I (high solubility, high permeability), the FDA allows a biowaiver-meaning no human bioequivalence studies are needed if the dissolution profile matches the brand-name drug exactly. This saves time and cost while maintaining safety.
Why is alcohol testing part of dissolution testing?
Some extended-release pills can release their entire dose too quickly if taken with alcohol-a dangerous effect called dose-dumping. Dissolution tests now include alcohol (up to 40% ethanol) to simulate this risk. If the drug releases too fast under these conditions, the product is rejected.
What happens if a generic drug’s dissolution profile changes after approval?
Any change to the manufacturing process, ingredients, or site requires retesting under the FDA’s SUPAC guidelines. If the dissolution profile shifts outside acceptable limits, the FDA can halt production until the issue is resolved. This ensures ongoing quality even after approval.