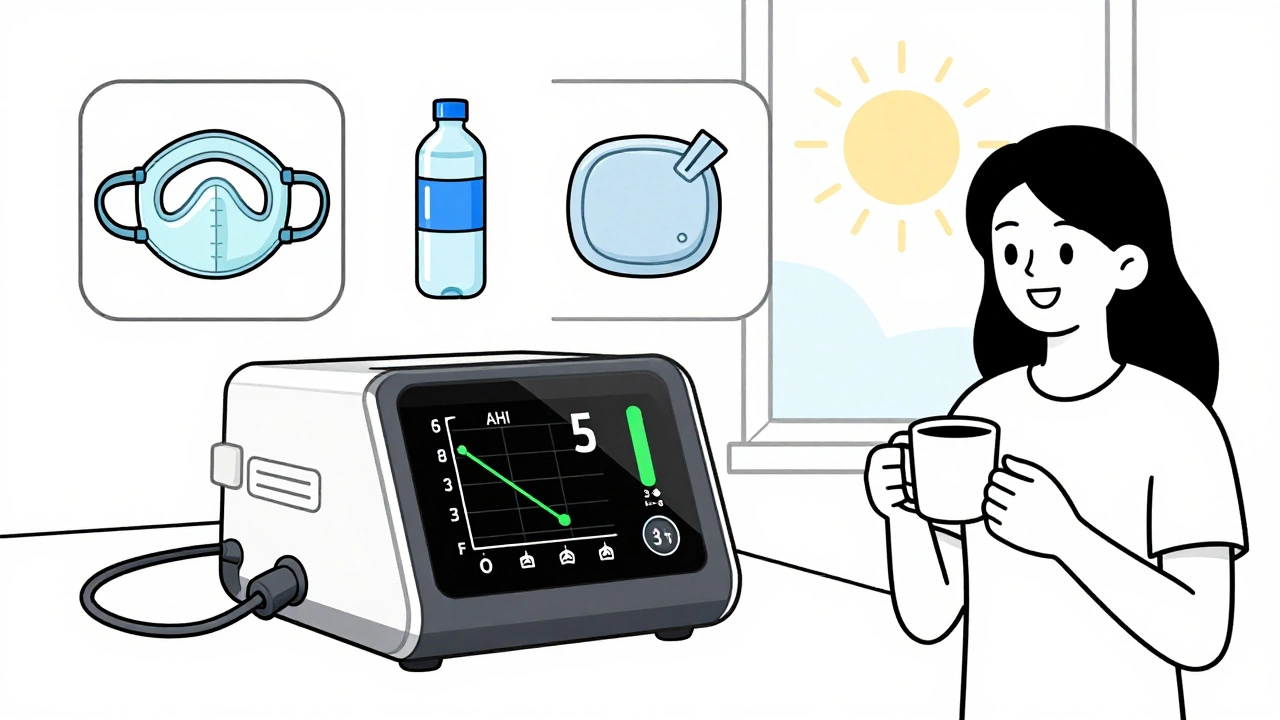
Waking up with a dry mouth, hearing air hiss from your mask, or feeling like the pressure is too high - these aren’t just annoyances. They’re red flags that your CPAP therapy isn’t working the way it should. If you’re using a CPAP machine and still tossing and turning, you’re not alone. About 42% of users deal with dry mouth, 58% struggle with mask leaks, and 31% say the pressure feels off. The good news? Most of these problems have simple, proven fixes. You don’t need to quit CPAP. You just need to fix what’s broken.
Dry Mouth? It’s Probably Not the Humidifier
Most people assume dry mouth means their humidifier isn’t working hard enough. But here’s the truth: dry mouth is almost always caused by mouth breathing during sleep, not low humidity. A 2023 study from the American Thoracic Society found that 67% of users who complained of dry mouth were breathing through their mouths while asleep - even with the humidifier turned all the way up. Your CPAP machine blows air into your nose. If your mouth is open, that air escapes, drying out your throat. The humidifier can’t keep up. You might even wake up with a sore throat, cracked lips, or a sticky feeling that makes you dread bedtime. Here’s how to fix it:- Switch to a full-face mask. This covers both your nose and mouth. One Reddit user, u/SleepSeeker2020, said their dry mouth vanished within three nights after switching from a nasal mask to a full-face mask.
- Use a chin strap. This simple device holds your jaw closed. About 45% of mouth breathers use one, and 38% report immediate relief. Look for adjustable, breathable models - not the stiff, uncomfortable ones.
- Turn up your humidifier. Even if mouth breathing is the main issue, a higher humidifier setting helps. Set it between level 3 and 4 on a 0-6 scale. Too high (level 5-6) can cause condensation in the tube - that’s water pooling, not better moisture.
- Use heated tubing. Heated tubes keep the air warm from the machine to your mask. Philips’ 2022 clinical trial showed heated tubing reduces dry mouth by 32% compared to standard tubing.
Mask Leaks? It’s Likely a Fit Issue
If you hear a loud hiss or wake up with red marks on your face, you’ve got a leak. Leaks aren’t just annoying - they waste air, reduce therapy effectiveness, and can trigger false alarms on your machine. Dr. David White from Harvard says leaks over 24 L/min seriously hurt treatment. That’s not a tiny drip - it’s a major escape. Most leaks happen because the mask doesn’t fit right. Not because it’s broken. Here’s how to fix it:- Check your cushion. Silicone cushions wear out. Replace them every 3 months. Even a tiny crack or flattening can cause leaks. Most DME providers say 92% of leak issues are solved just by swapping the cushion.
- Adjust the headgear. Don’t crank it tight. Over-tightening causes leaks by distorting the seal. Try the airflow test: turn on your CPAP, then gently pull the mask away from your face until you hear the hiss. Slowly push it back until the sound fades. That’s your sweet spot.
- Don’t sleep on your stomach. Side and back sleepers get fewer leaks. If you’re a stomach sleeper, your face is pressed into the pillow, crushing the mask. Try a CPAP-friendly pillow with cutouts for the mask.
- Try a different mask style. If nasal pillows leak constantly, try a nasal mask. If a nasal mask leaks at the bridge of your nose, try a full-face. Your face shape matters. ResMed’s AirFit F30i and Philips’ DreamWear are two of the most leak-resistant designs on the market.
Pressure Too High? Or Too Low?
Pressure settings are the most misunderstood part of CPAP therapy. Many users are set at a fixed pressure that was determined during a sleep study - but your needs change. You might gain weight, lose weight, or develop allergies. Your pressure might be too high, causing chest discomfort, or too low, letting apneas sneak back in. Dr. Nancy Collop from Johns Hopkins says pressure adjustments below 5 cm H₂O can improve comfort without losing effectiveness. That’s a tiny tweak - but it makes a huge difference. Here’s what to do:- Don’t adjust pressure yourself. Most machines let you change pressure by ±2 cm H₂O, but doing so voids your warranty and risks poor treatment. ResMed’s 2023 policy is clear: only a sleep specialist should adjust pressure.
- Ask for an APAP machine. If you’re on a fixed-pressure CPAP, ask your doctor about switching to an auto-adjusting model (APAP). These machines read your breathing every 5-10 seconds and adjust pressure on the fly. ResMed’s AirSense 11 AutoSet and Philips’ DreamStation 2 do this well. Users report 4.2/5 stars for comfort compared to 3.8/5 for fixed-pressure models.
- Use expiratory pressure relief. This feature lowers pressure slightly when you breathe out. It’s called EPR (ResMed), C-Flex (Philips), or EZ-Ex (Fisher & Paykel). It makes breathing feel more natural. One Reddit user, u/ExhaustedEngineer, said his chest pain disappeared after switching from 14 cm H₂O to 9 cm H₂O with EPR enabled.
- Check your data. Most modern machines track your apnea-hypopnea index (AHI). If your AHI is above 5, your pressure might be too low. If you’re consistently hitting the machine’s max pressure (usually 20 cm H₂O), it might be too low. Talk to your sleep specialist with the data.

When to Call Your Provider
Some problems need more than a mask swap or humidifier tweak. Call your sleep specialist if:- Your AHI stays above 5 after 30 days of consistent use.
- You’re leaking more than 24 L/min for more than 2 weeks - even after trying new cushions and headgear.
- You’re still waking up with dry mouth after trying a full-face mask and chin strap.
- You feel claustrophobic, anxious, or panic when wearing the mask.
Keep Your Machine Clean, Keep It Working
A dirty machine causes problems you might not even notice. Dust in the filter? That can reduce airflow and make your machine work harder. Mold in the water chamber? That’s a health risk.- Wash your mask and tubing weekly with mild soap and warm water. Let them air dry.
- Replace the water chamber every 6 months - even if it looks fine. Cracks and mineral buildup happen slowly.
- Change your filter every 30 days for foam, every 90 days for HEPA. ResMed’s manual says this keeps airflow clean and consistent.
- Use distilled water in the humidifier. Tap water leaves mineral deposits that clog the chamber and can damage the machine.
Stick With It - It Gets Better
Most people give up on CPAP in the first 3 months. But studies show 78% of users master basic troubleshooting within 14 days. The first week is the hardest. By week 3, most report better sleep, more energy, and fewer headaches. The goal isn’t perfection. It’s consistency. Even 4 hours a night helps. Medicare requires 4+ hours nightly for 70% of nights over 30 days to keep coverage. You don’t need 8 hours. You just need to show up. If you’re struggling, reach out. ResMed offers 24/7 support with a 97% same-day response rate. Your DME provider should be helping you, not just delivering equipment. You paid for therapy - not just a machine.What’s Next?
CPAP tech is getting smarter. New models like the ResMed AirSense 11 use AI to detect leaks as small as 12 L/min. The upcoming S+ algorithm (coming in Q2 2024) promises 23% better leak compensation. Apps like DreamMapper now give you personalized pressure tips based on your 30-day usage. But the real breakthrough isn’t in the machine. It’s in the user. When people stop seeing CPAP as a burden and start treating it like a tool - like a pair of glasses for sleep - everything changes. You don’t need to be perfect. You just need to be consistent. Fix the leaks. Stop the mouth breathing. Get the pressure right. Then sleep - deeply, quietly, and without fear.Why does my mouth get dry even with a humidifier on?
Dry mouth from CPAP is almost always caused by mouth breathing, not low humidity. When you breathe through your mouth, the pressurized air escapes and dries out your throat. A humidifier can’t compensate for open-mouth breathing. Switching to a full-face mask or using a chin strap solves this in most cases.
How do I know if my CPAP mask is leaking?
You’ll hear a loud hissing sound, see your machine’s leak alert light up, or wake up with red marks on your face. Use the airflow test: turn on your CPAP, gently pull the mask away until you hear air escape, then push it back slowly until the sound stops. That’s the right seal. Leaks over 24 L/min reduce treatment effectiveness.
Can I adjust my CPAP pressure myself?
Most machines let you change pressure by ±2 cm H₂O, but doing so voids your warranty and risks poor treatment. Pressure settings should be determined by a sleep specialist based on your sleep study results. If you feel the pressure is too high or low, ask for an APAP machine or a pressure titration study - don’t adjust it on your own.
How often should I replace my CPAP mask cushion?
Replace your mask cushion every 3 months. Silicone breaks down over time from oils on your skin, cleaning, and daily use. Even small cracks or flattening can cause leaks. Most DME providers say 92% of leak problems are solved just by replacing the cushion.
What’s the difference between CPAP and APAP?
CPAP delivers a fixed pressure all night. APAP (auto-adjusting) changes pressure automatically based on your breathing - lowering it when you’re calm, raising it when you snore or have an apnea. APAP is better for people whose needs change, like those who gain/lose weight or have variable sleep patterns. ResMed’s AirSense 11 AutoSet and Philips’ DreamStation 2 are popular APAP models.
Is it normal to still have apneas with CPAP?
You should have fewer than 5 apneas per hour (AHI under 5) with effective CPAP therapy. If your AHI stays above 5 after 30 days of consistent use, your pressure might be too low, your mask might be leaking, or you might need a different therapy. Check your machine’s data and talk to your sleep specialist.
Can CPAP cause sinus problems?
CPAP itself doesn’t cause sinus problems, but dry air, dirty equipment, or pressure that’s too high can irritate your nasal passages. Using a heated humidifier, cleaning your mask weekly, and using saline spray before bed can help. If you get frequent sinus infections, ask your doctor about switching to a full-face mask or adding a nasal steroid spray.






15 Comments